This content is also available in:
Italiano
Português
Čeština
Română
Benign cell content of cytological preparations
A cervical smear or liquid-based cytology (LBC) preparation that has been correctly taken with a spatula, broom or brush will contain a variety of epithelial cells from the non-keratiising squamous epithelium, transformation zone and endocervical canal as described in the section on anatomy, histology and function of the uterine cervix.
A benign cervical smear or LBC slide will contain:
Squamous epithelial cells from the ectocervix
- Superficial squamous cells
- Intermediate squamous cells
- Parabasal squamous cells
- Navicular cells
Columnar epithelium from the endocervical canal
- Endocervical cells
Metaplastic squamous cells from the transformation zone
Commensal vagina flora
- Lactobacilli, Gardnerella vaginalis, Leptothrix vaginalis
Cervical mucus
A benign cervical smear or LBC slide may contain
Exfoliated endometrial cells (dependant of stage of menstrual cycle)
- Epithelial cells
- Superficial stromal cells
- Deep stromal cells
Histiocytes, leucocytes, and red blood cells
Contaminants
- e.g. spermatozoa, talc granules
Basic cytological pattern
The type of epithelial cells seen in a cervical smear is determined by:
- The degree of maturation of the cervical epithelium
- The location of the squamocolumnar junction
- The presence of metaplastic change in the transformation zone
- The stage in the menstrual cycle when the smear is taken
- The effect of hormones in pregnancy or ingested oral contraceptives or hormone replacement therapy
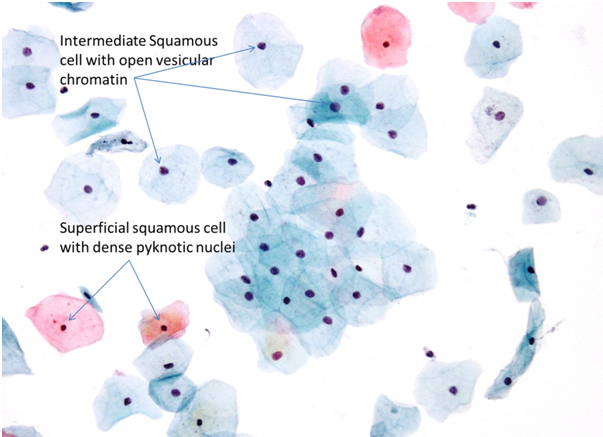
Superficial squamous cells
Large polygonal shaped cells ranging from 40 60 microns in size with central pyknotic nuclei and abundant translucent eosinophilic/cyanophilic cytoplasm, which may contain keratohyaline granules. In cervical smears or LBC slides, superficial squamous cells generally present as discrete single cells.
Intermediate squamous cells
Similar size to superficial squamous cells, intermediate cells have slightly larger central vesicular nuclei with a fine, even chromatin pattern and abundant transparent cyanophilic/eosinophilic cytoplasm. The intermediate squamous cells can present singly or in clumped cell groups.
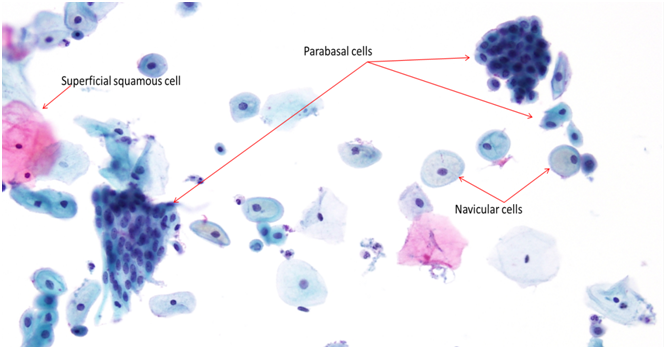
Navicular cells, representing a variant of intermediate cells, often present in pregnancy or post-partum. The cells are boat shaped with a thickened outer rim of cyanophilic/eosinophilic cytoplasm and eccentric nuclei. Central cytoplasmic brown/yellow staining indicates glycogen production.
- Navicular cells are seen with high progesterone levels when superficial squamous cells exfoliate more readily: thus they may be seen with progesterone-only contraceptive use.
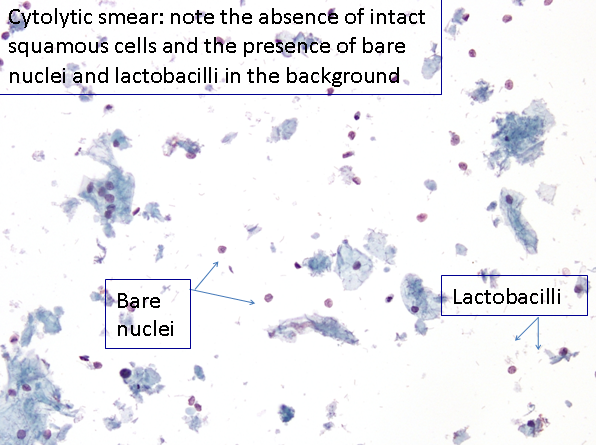
- Intermediate cells often undergo cytolysis. This is a normal physiological process in the presence of lactobacilli particularly seen late in the cycle or with progesterone-only contraceptive pills. It results in bare nuclei in the smear or LBC slide.
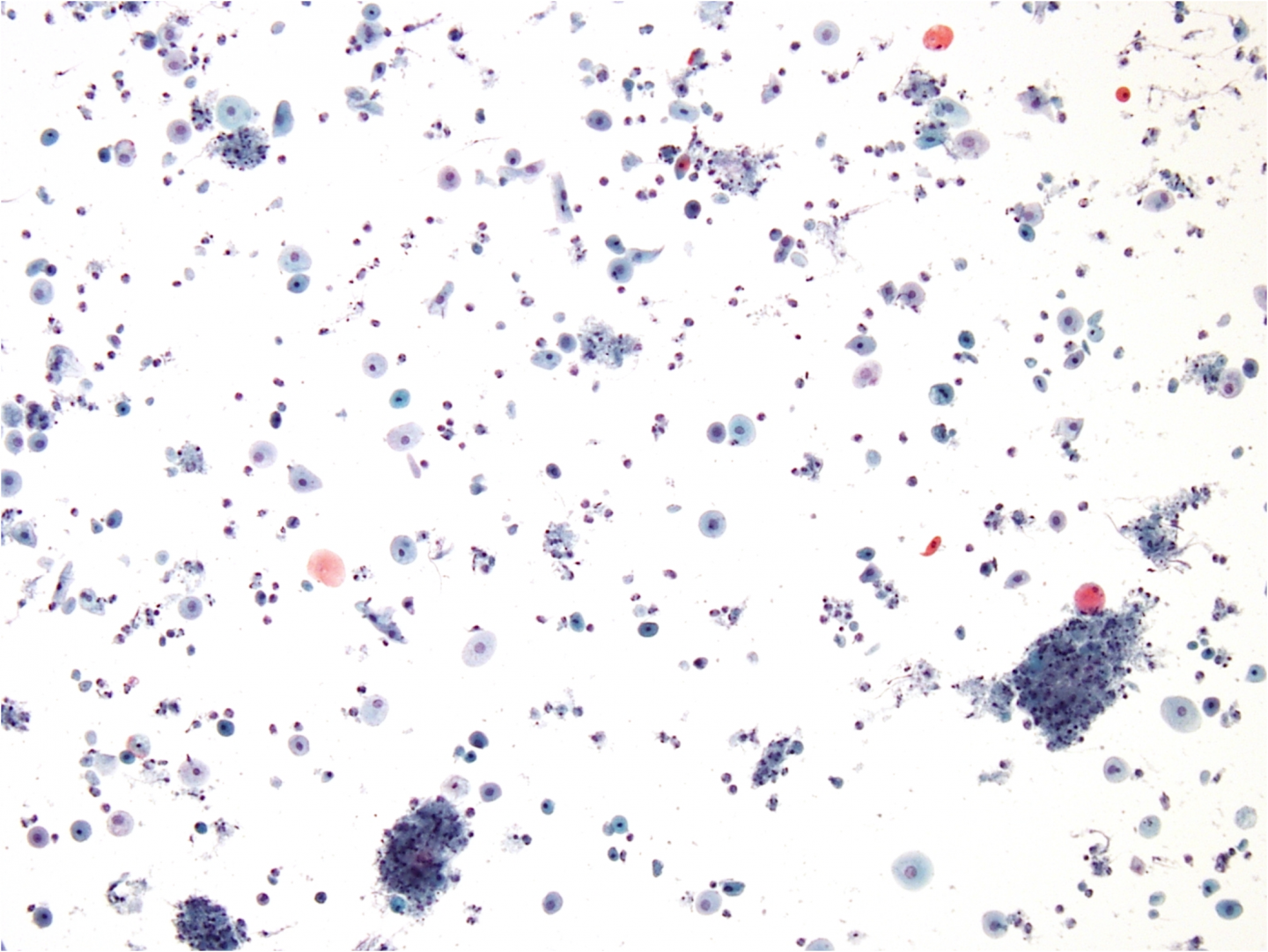
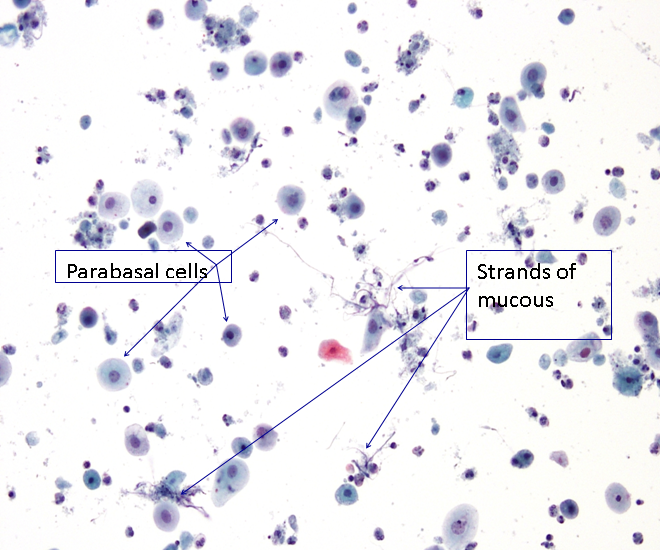
Parabasal squamous cells
Parabasal squamous cells are small oval to round immature squamous cells. The cells have a large central vesicular nucleus with fine even chromatin and a dense cyanophilic cytoplasm. The cells can be seen both singly and in groups.
Anucleate squamous cells
Anucleate squamous cells are exactly that, squamous cells with no nucleus. These are not normally exfoliated from the cervix or vagina, but are present in the lower third of the vagina and vulva, their presence in a cervical smear may indicate:
· Parakeratosis and hyperkeratosis (leukoplakia) of the ectocervix.
· Contamination of the cervical smear from sampling the vulva or lower third of the vagina.
· Inflammatory response.
· Ruptured foetal membranes i.e. anucleate foetal squames.
· The sample is a vulval smear.
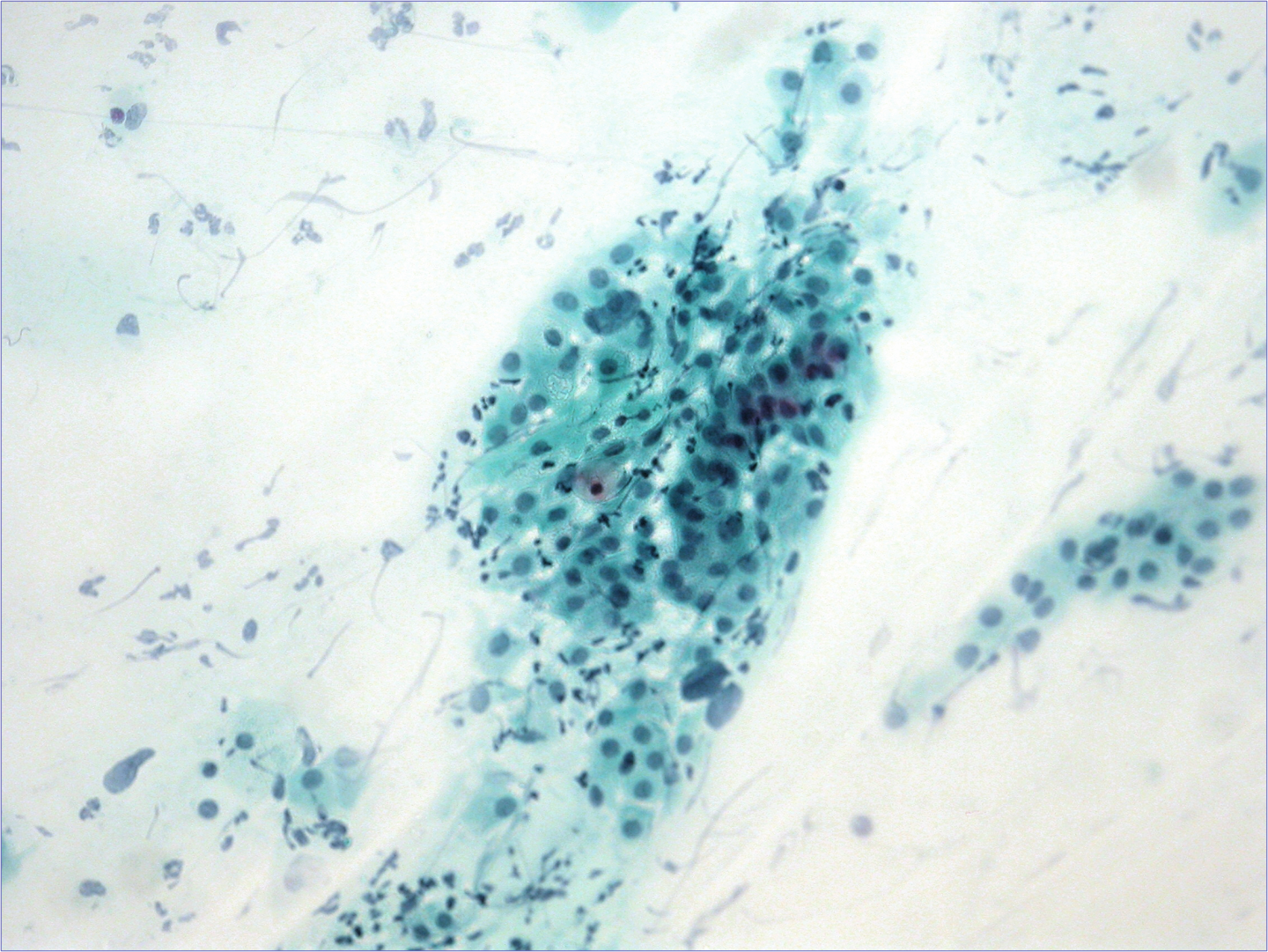
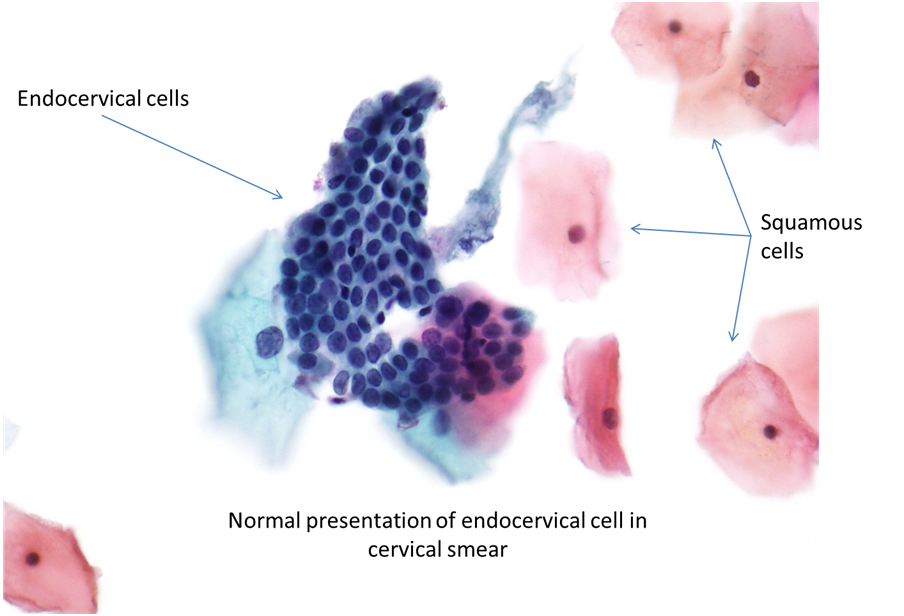
Endocervical cells
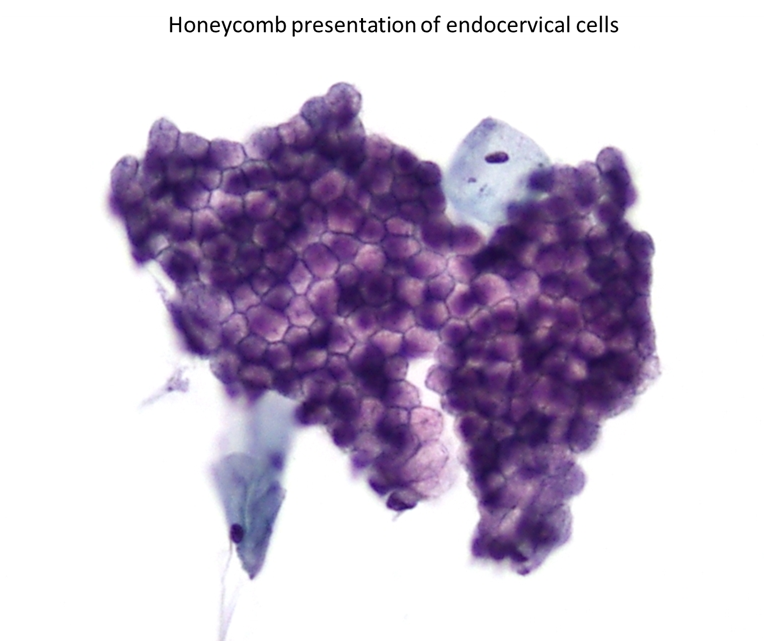
Endocervical cells are the epithelial cells of the endocervix. These may be shed singly, in strips forming a palisade picket fence or as flat sheets with a very regular architecture. Occasionally, the honeycomb effect may be visualised in flat sheets of endocervical cells containing abundant mucous. The nucleus is situated basally with evenly distributed fine to granular chromatin. Multinucleation and increased nuclear size is often seen in infection, including human papillomavirus (HPV) infection and pregnancy. The cells are columnar and symmetrical across their longitudinal plane. The cytoplasm is described as delicate and is often vacuolated and may contain a cytoplasmic tail, the remnant of the cells basement membrane attachment.
Metaplasia
Early metaplasia
Early metaplastic cells are formed from basal/reserve cell proliferation. Early metaplastic cells are not exfoliated, so if they are present in a cervical smear, they will have been directly sampled. Due to the direct sampling, early metaplastic cells will appear as tissue fragments. The cells are small with a high N:C ratio, they have fine, evenly distributed chromatin, a well defined thin, even nuclear membrane and may still be attached to adjacent endocervical cells.
Immature squamous metaplasia
Immature metaplastic cells can appear in cervical smears as single cells or in sheets (single presentation often seen in LBC, due to mechanical agitation). Immature metaplastics have a tendency to retain a slight columnar shape (transforming from glandular to squamous cell), they have a high nuclear:cytoplasmic (N:C) ratio with coarse granular chromatin and contain prominent eosinophilic nucleoli. Mitotic figures can seldom be seen.
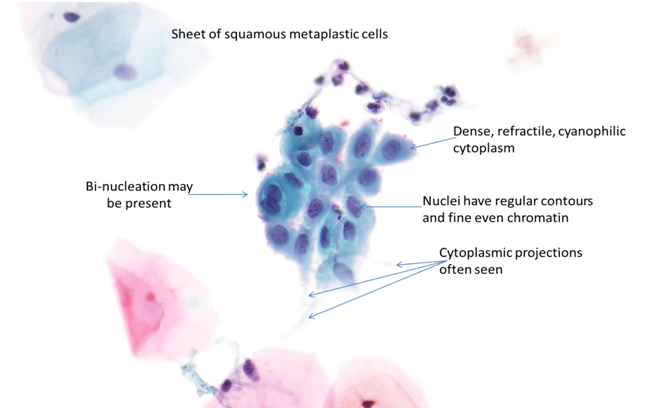
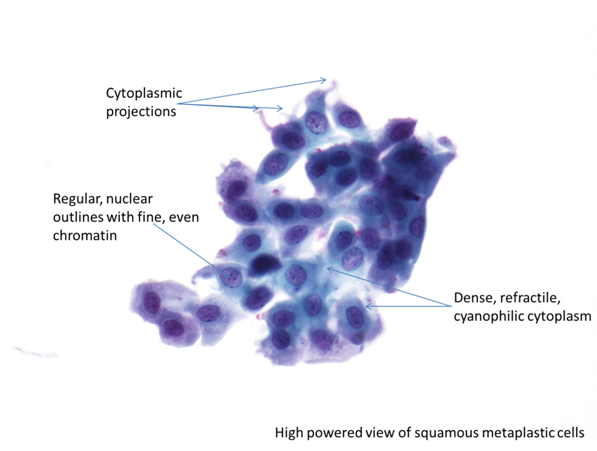
Mature squamous metaplasia
Mature squamous metaplastic cells are oval to polygonal in shape (transformed to a squamous type cell); they have sharp cytoplasmic borders with dense cyanophilic cytoplasm. Intercellular bridges may be visualised as cytoplasmic fingers or projections. When seen singly or in sheets, mature metaplastic cells, can be difficult to differentiate from parabasal cells.
Sampling the transformation zone
If the transformation zone (TZ) is sampled correctly, there will be endocervical cells or squamous metaplastic cells in the cervical smear. The screener will need to take into consideration the age and hormonal status of the patient being screened as the position of the squamocolumnar junction (SCJ) varies in its positions throughout the reproductive life of the female.
Normally a cervical smear will contain anywhere between one and 10 groups of endocervical cells (a group should be a cluster of 10 cells), one group is often enough to indicate that the transformation zone has been sampled.
After menopause, the SCJ recedes into the canal endocervical canal beyond the reach of the brush, broom or spatula and so smears taken after the menopause rarely contain endocervical cells. Smears taken in the presence of ectropion contain abundant benign endocervical cells. Immature metaplastic cells are found in young women of child bearing age or following treatment to the cervix, they are rare in smears from older women.
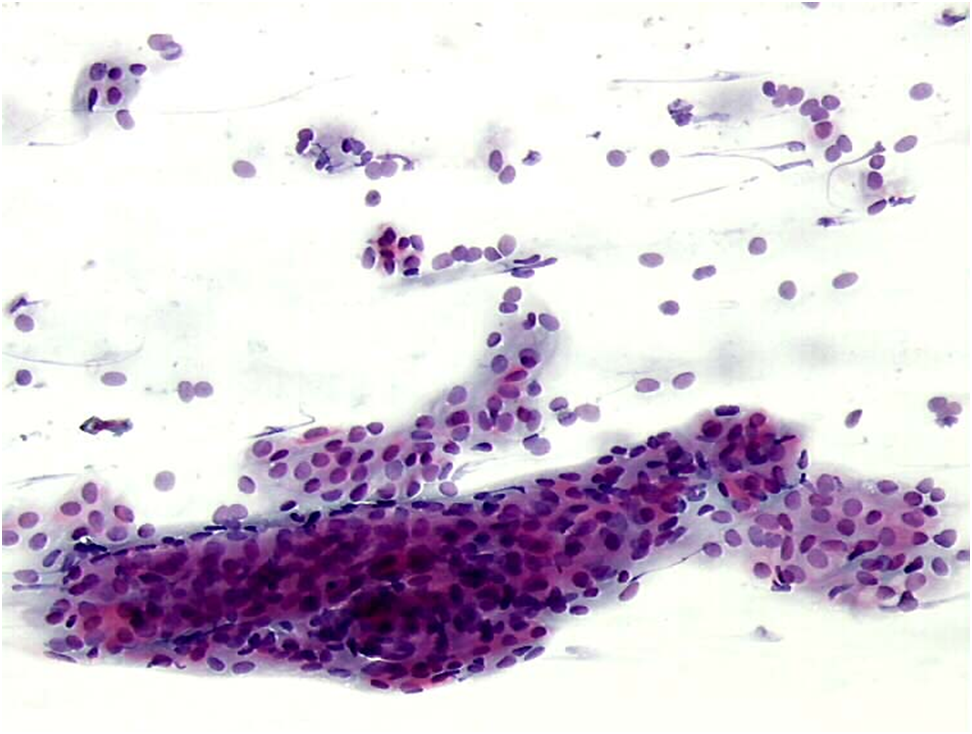
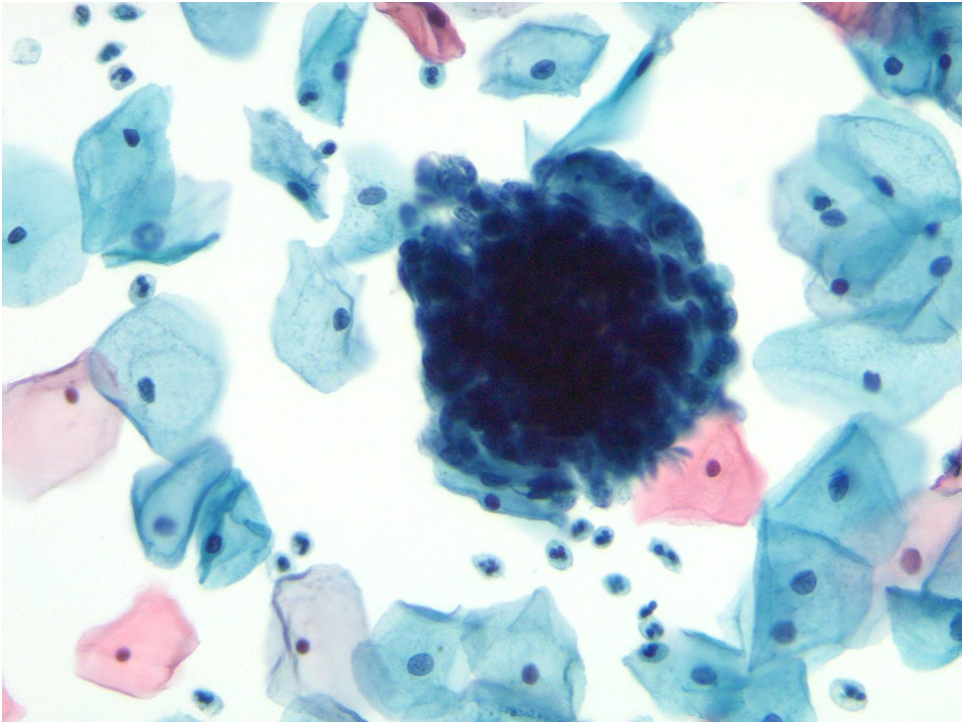
Figure 9b-4 (a-d). Transformation zone sampling
Endometrial cells
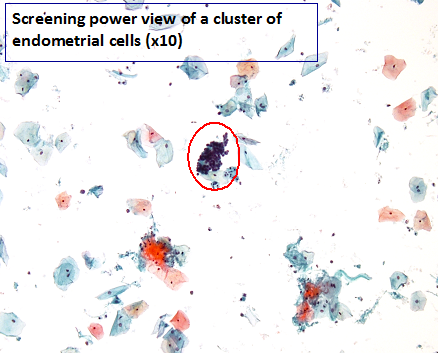
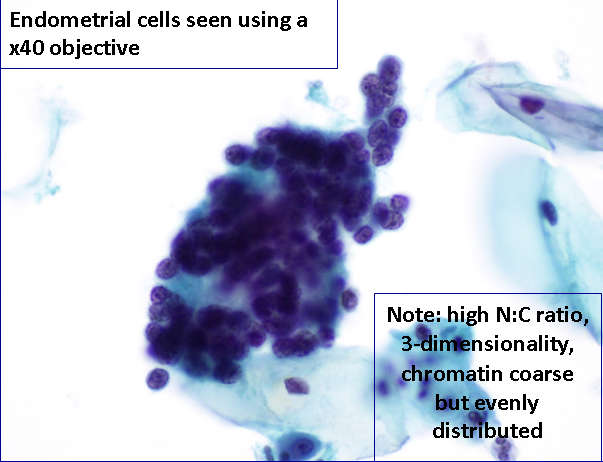
Endometrial cells should theoretically be shed around days 0-12 of the menstrual cycle but depending on certain physiological and pathological changes such as dysfunctional uterine bleeding, endometrial polyp, endometrial hyperplasia, intrauterine contraceptive device (IUCD) or well differentiated endometrial carcinoma they may be seen at any time.
Epithelial cells can be exfoliated singly or in 3-dimentional clusters often referred to as mulberry formations. Endometrial cells have a high N:C with delicate cyanophilic cytoplasm (at times difficult to visualise). The nuclei have coarse, evenly distributed chromatin and a single small nucleolus.
Unless the typical 3-dimensional appearance is seen, these cells may be confused with hyperchromatic crowded groups of cells in high-grade squamous intraepithelial lesions especially with CIN3. [Link to Chapter 10 Pitfalls]
As the presence of endometrial cells can be an indicator of pathology in a post-menopausal woman, their presence should be discussed, and further investigation should be advised to the smear taker.
Figure 9b-5 (a-c)
The post-menopausal smear
The menopause is associated with diminishing oestrogen activity which is reflected in the smear cervical smear pattern as the mature multi-layered epithelium is replaced by the immature atrophic epithelium. Smears usually contain parabasal cells either as discrete rounded cells or as sheets of cells. Bare nuclei (nuclei striped of cytoplasm) may also be present. Infection and/or inflammatory changes are common. The presence of endocervical cells in a post-menopausal smear is diminished because of the inversion of the transformation zone. Inversion causes the endocervical area to move deeper into the endocervical canal where sampling can be out of reach of the spatula/brush.
In atrophic smears, where there is some doubt in the diagnosis, it may be useful to administer a short course of topical oestrogen therapy to the patient and repeat the smear within 90 days when a low proliferative pattern may be seen.
Figure 9b-6 a-d. Typical atrophic cell pattern