Squamous intraepithelial lesion (SIL)
The histological spectrum of CIN is described cytologically as squamous intraepithelial lesion (SIL) is primarily recognised by the abnormal chromatin pattern and nuclear membrane irregularity as described in Table 9c-1 above and referred to in the UK system as ‘dyskaryosis’. The distinction between high-grade and low-grade (HSIL and LSIL) depends on the degree of nuclear and cytoplasmic maturation as demonstrated by nuclear/cytoplasmic (NC) ratio, which will be expressed in this chapter as a percentage: i.e. nucleus/cytoplasmic diameter of 0.9/3.6 = 25%.
Apart from the distinction between benign/reactive and SIL/dyskaryosis, the most critical distinction is between LSIL and HSIL because this affects decisions for patient management and the necessity for treatment.
| Principles to remember:A cytological diagnosis is a prediction of what is going to be seen on a histological resection specimen or biopsyThe diagnosis of SIL on cytology depends on an abnormal nuclear chromatin pattern and irregular nuclear membrane.The histological diagnosis of CIN1-3 relates to the degree of maturation of abnormal cells in the squamous epithelium and is reflected in cytology by the nuclear/cytoplasmic ratio |
Figure 9c-1. Schematic representation of the development of CIN (taken from Figure 1 in Kelloff & Sigman 2007)
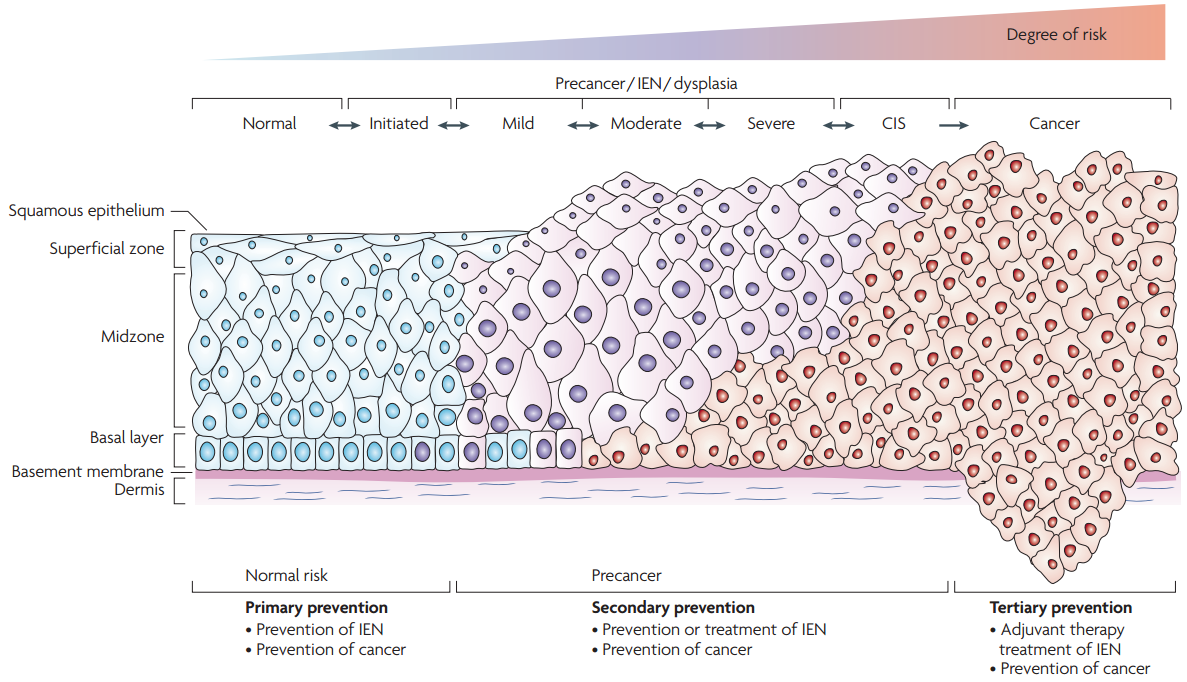
Four important features of SIL/dyskaryosis and the degree of abnormality.
- Discrepancy between nuclear and cytoplasmic maturation
- Nuclear membrane irregularity
- Irregular chromatin distribution and increased granularity
- Increasing nuclear/cytoplasmic (NC) ratio
Low-grade squamous intraepithelial lesion (LSIL)
Presentation
The cells will appear on the cervical smear as mature cells that are polygonal in shape as are normal intermediate or superficial cells. LSIL can present both singly and in sheets but mainly as single cells.
Nucleus
The nucleus is enlarged but most importantly there is an abnormal chromatin pattern. There is increased chromatin granularity although it may remain evenly distributed in LSIL. The UK classification recognises that dyskaryosis, i.e. abnormal chromatin pattern, is a feature of all grades of SIL (Denton et al. 2008). The nucleus is usually hyperchromatic and the nuclear outline irregular but less so than in HSIL. Bi/multinucleation may be present. There are no nucleoli associated with LSIL.
Cytoplasm
The cytoplasm is cyanophilic or eosinophilic depending on the maturation of the cell and has a similar density to that of a normal intermediate squamous cell. The mean cytoplasmic area/ diameter has been shown to be lower than that of a normal intermediate cell (Slater et al. 2005a).
Dyskeratosis (intracytoplasmic keratinisation) and parakeratosis may be seen in LSIL, which should lead to a search for features elsewhere suggesting HPV infection. Keratinisation should lead to a search for evidence of HSIL or even cancer.
Nuclear/cytoplasmic ratio
The main feature distinguishing LSIL from HSIL is the NC ratio. The NC ratio can be assessed on area or diameter of the cells and has been shown to be significantly different between normal intermediate cells, LSIL and HSIL largely because of decreasing mean diameter of the cytoplasm rather than increasing size of the nucleus (Slater et al. 2005a; 2005b). On the whole, the diameter is easier to assess morphologically.
In their morphometric study of TBS and BSCC criteria using conventional as well as liquid-based cytology (ThinPrep and SurePath), Slater et al. (2005a and b) proposed, as a guide based on mean diameter of the nucleus and cytoplasm, a NC ratio for LSIL less than 50%, 50% or more for HSIL and 25% for a normal intermediate cell.
| Morphometric criteria for NC ratio based on mean diameter % (Slater et al. 2005a and 2005b)Normal intermediate cell 25%LSIL (mean 40%) <50%HSIL (mean 60%) >50% |
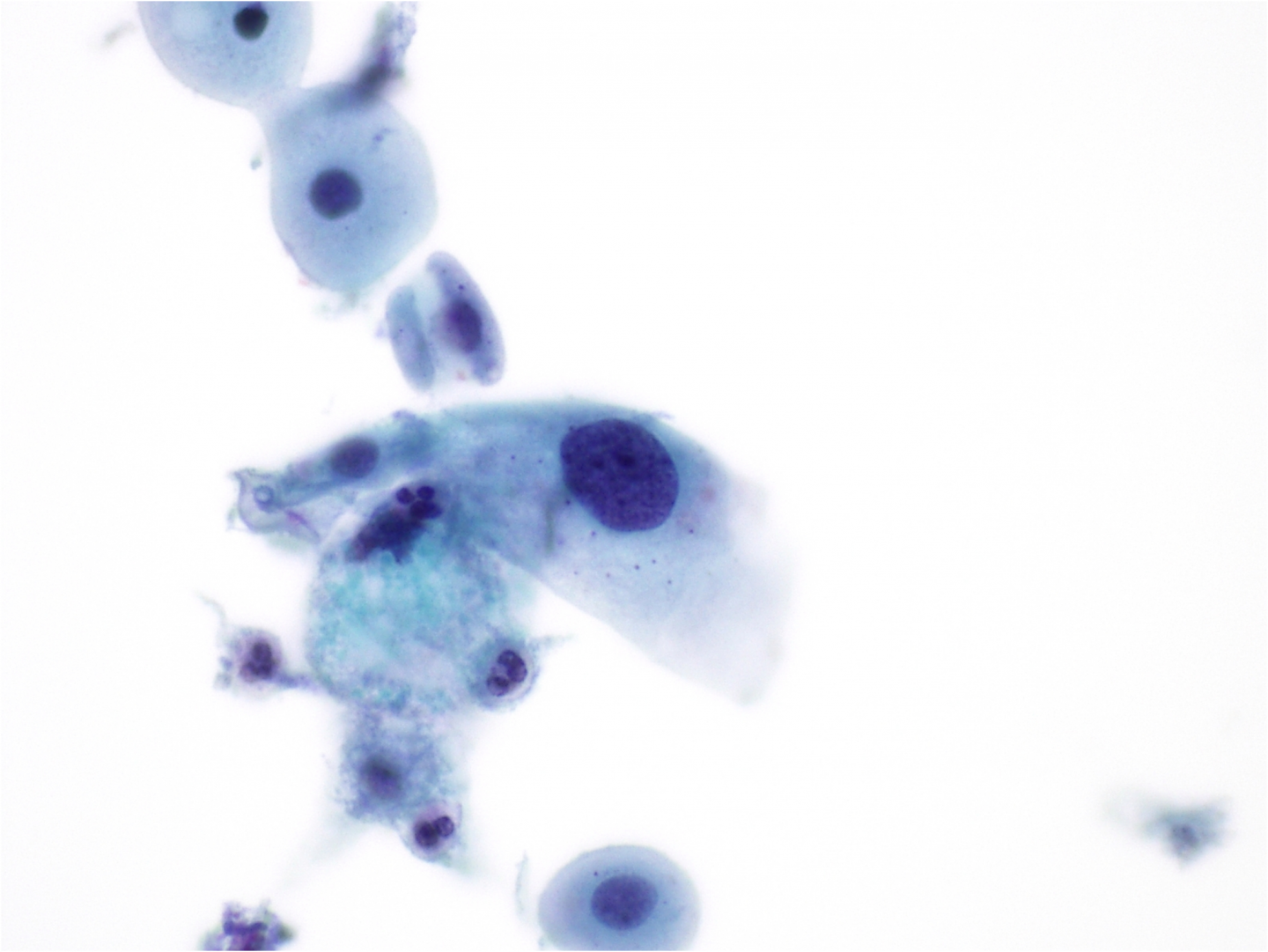
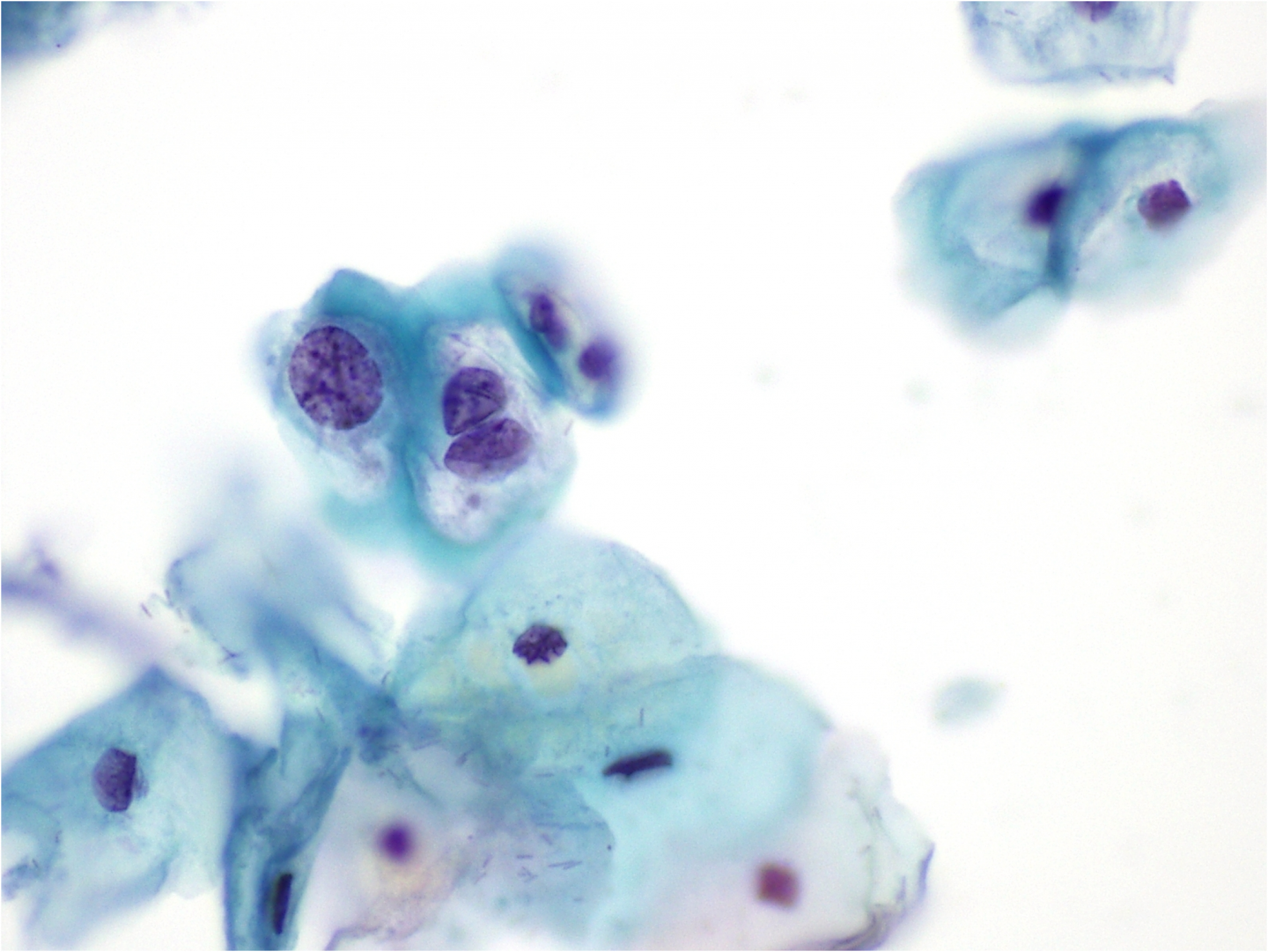
Figure 9c-2 (a-c). Low-grade squamous intraepithelial lesion (SIL)
(a) Increase in NC ratio in SIL (40% in this cell): the cell has matured to the size of a normal intermediate cell. The nucleus is still fairly round in shape; chromatin is coarser than normal and hyperchromatic.
LSIL and HPV infection
LSIL is caused by HPV infection, which in most instances is reversible. LSIL often shows features of productive HPV infection – particularly koilocytosis, which is its morphological hallmark.
| Koilocytosis and its relationship to LSILKoilocytosis is a feature of productive infection by HPV but cannot reliably be distinguished from CIN1 either on histology or cytologyIt is impossible to be certain from histology, cytology or HPV testing whether a productive infection will persist or progress rather than regressLow-risk and high-risk HPV cannot reliably be distinguished by cytology or histologyThe majority of LSILs are caused by HPV whether or not koilocytosis is present. |
Cytological features of koilocytes
- Cells that are infected by and exhibit the cytopathic effects of HPV are known as koilocytes.
- Koilocytes MUST exhibit both nuclear and cytoplasmic criteria for the diagnosis to be made.
- Generally, koilocytosis occurs in the intermediate and superficial layers of the squamous epithelium, thus the cell size should be similar to that of intermediate and superficial squamous cells.
- Koilocytes are considered as a feature of LSIL in TBS (Nayar & Solomon 2004; Wilbur et al. 2015) and the UK system (Denton et al. 2008) since the distinction between HPV infection and CIN1 cannot be made reproducibly.
- Koilocytes are most often seen with LSIL but may also be seen in HSIL
Cytoplasmic criteria
- There is a circumscribed area of clearing around the nucleus known as a koilocyte (koilos means ‘hollow’ in Greek’). This area of clearing is, when examined ultrastructurally, filled with viable virus particles.
- A thick cytoplasmic rim is present around the vacuole representing margination of the cytoplasmic contents.
- As with LSIL, the cytoplasmic diameter is likely to be smaller than a normal intermediate cell.
Nuclear criteria
- There may be a single nucleus, binucleation or multinucleation.
- Loss of rounded nuclear contours with nuclei displaying straight, sharp edges.
- A slight a degree of enlargement of the nucleus as well as changes to chromatin distribution throughout the nucleus.
- Chromatin may appear blurred (in keeping with the viral nature of the infection) or vesicular with a fairly uniform appearance, although it is coarser than normal.
Koilocytosis may involve parabasal and metaplastic cells, which must be taken into account when small cells appear koilocytic.
Nuclear criteria
- The nuclear criteria are the same as previously described
- As the infected cells are immature, the NC ratio is higher.
Cytoplasmic criteria
- Instead of having large ‘caves’ of cleared cytoplasm, the immature cells will display perinuclear clearing with sharply defined halos.
- The halo is larger than would be expected with non-specific inflammation
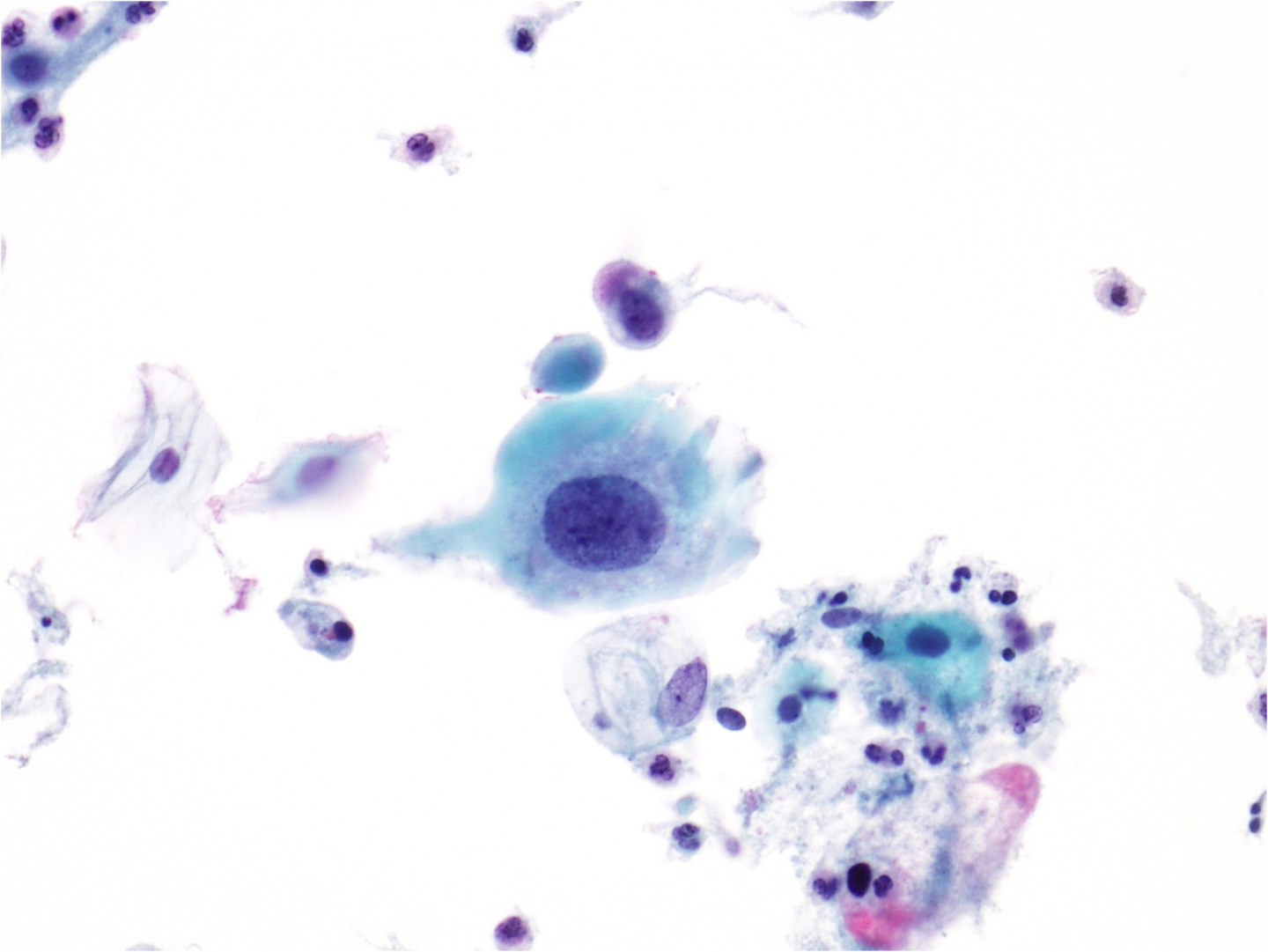
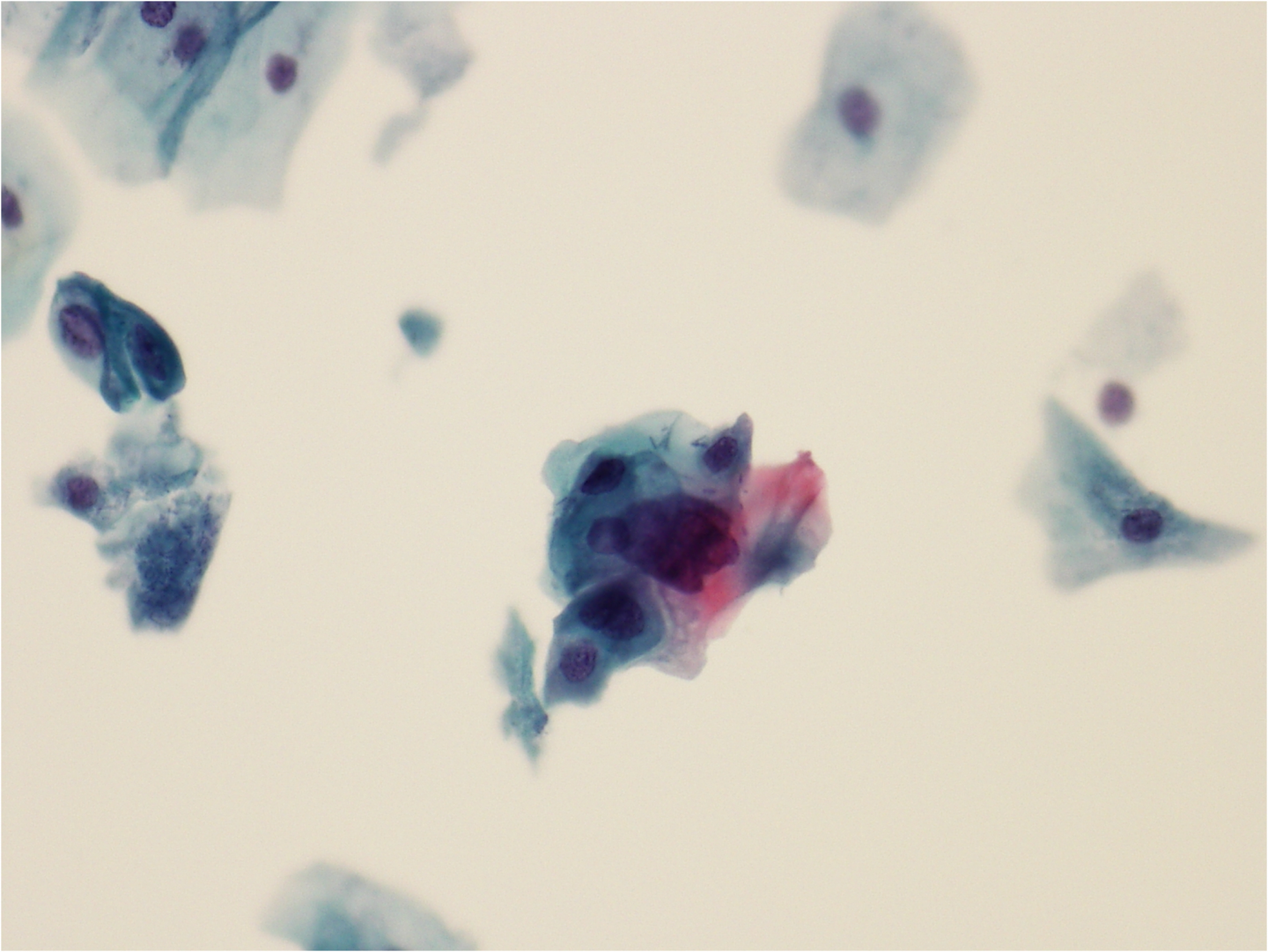
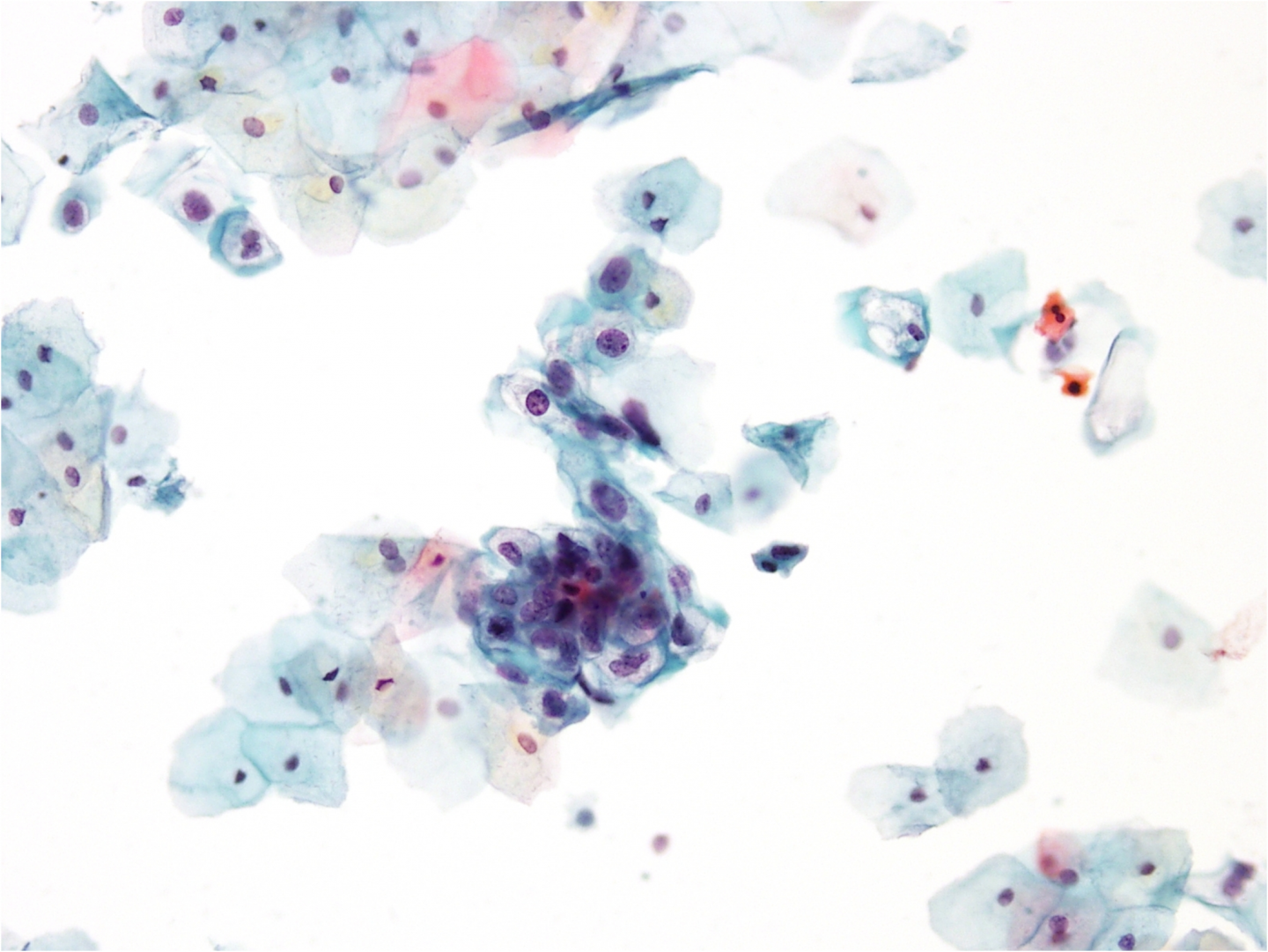
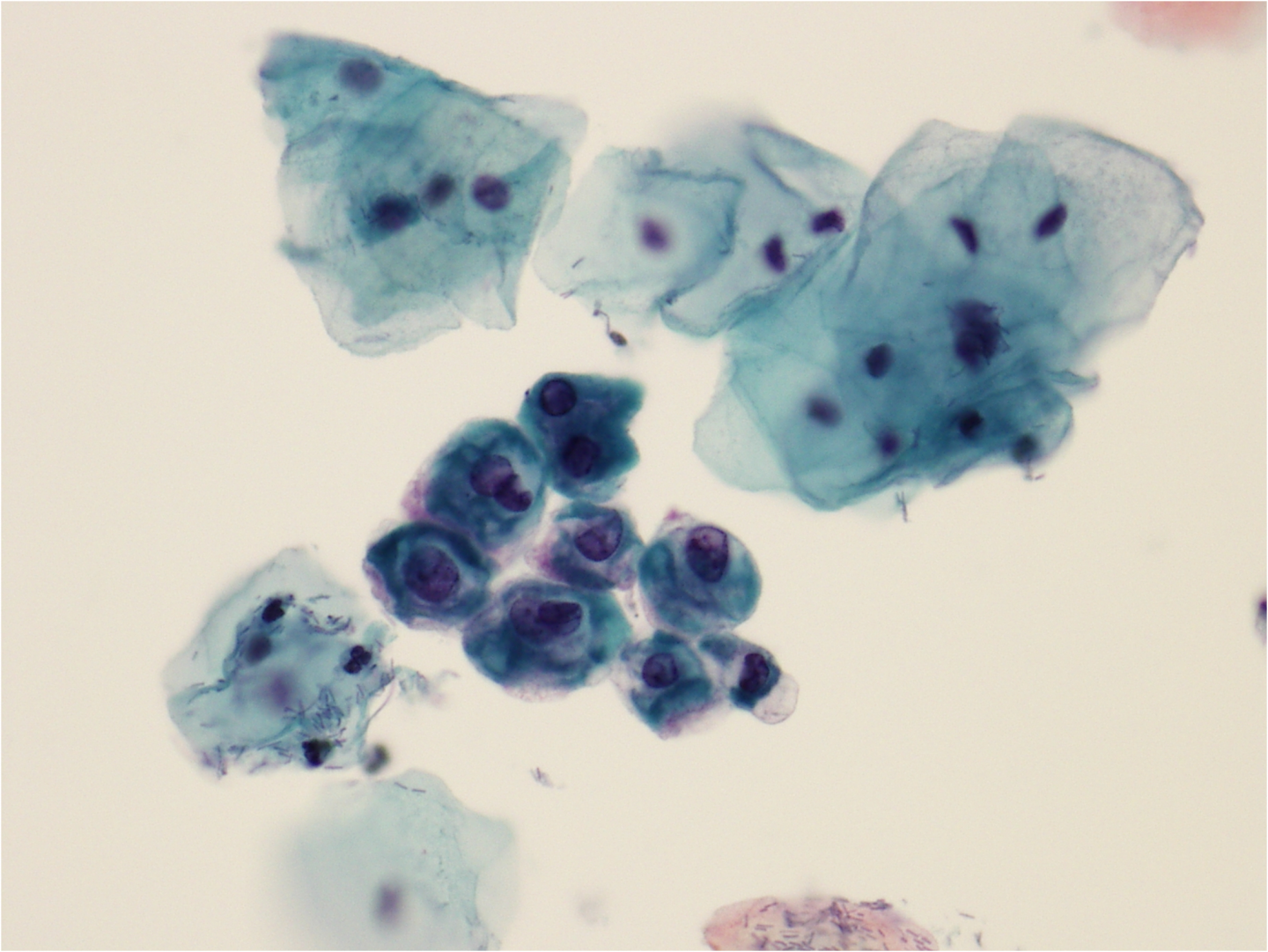
Figure 9c-3 (a-c). Koilocytosis.
(a) Koilocytosis involving a sheet of intermediate cells in LSIL