This content is also available in:
Italiano
Português
Čeština
Română
Vaginal microbiology
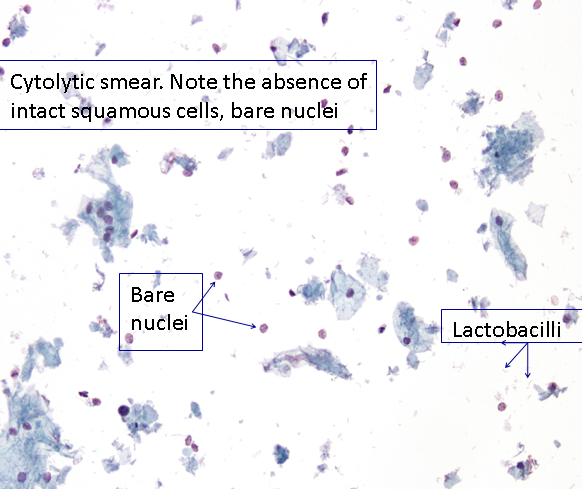
In cytology we are able to visualise a wide range of organisms, and in the case of viruses, we are able to see their cytopathic effects. Physiologically, the vaginal vault contains a mixture of both aerobic and non-aerobic bacteria, most importantly lactobacilli, which helps to maintain an acid environment, usually around pH 4.5. In the secretory phase of the menstrual cycle and pregnancy, the bacilli are associated with cytolysis. Clinically this may be associated with an odourless white/clear vaginal discharge.
Specific infections of the cervix
The inflammatory changes described above are common to almost all cases of acute cervicitis. In some cases the actual microbiological organism can be identified on the slide or will produce a distinctive cytopathic effect allowing the cytotechnologist to make a diagnosis on the infective organism.
Specific infective agents that are reported in cytology are:
- Trichomonas vaginalis
- Candida albicans
- Herpes simplex virus
- Human papillomavirus
- Actinomyces sp.
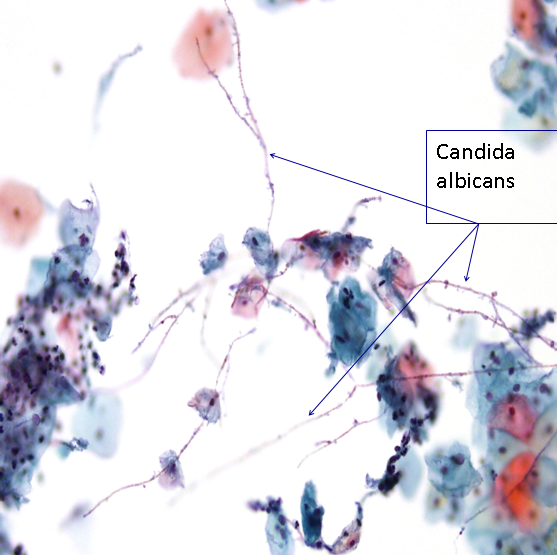
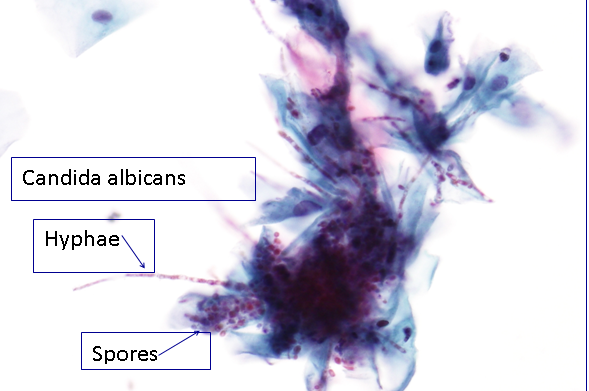
Thrush or Candidiasis is caused by Candida albicans. Clinically it presents with a white, curdled odourless discharge and can be associated with vulvar itching. In cytology we report the presence of both hyphae and spores even if it is not clinically suggested. Generally speaking, candida can be seen in smears from any patient, at anytime of the menstrual cycle, at any age and with or without symptoms. Non-specific inflammatory changes may be seen (see the section below). Perinuclear vacuoles are commonly seen as well as parakeratosis (orangeophilia of superficial and intermediate cells).
Candida may be seen on a scanned LBC slide
Figure 9b-8 (a-b). Candida albicans
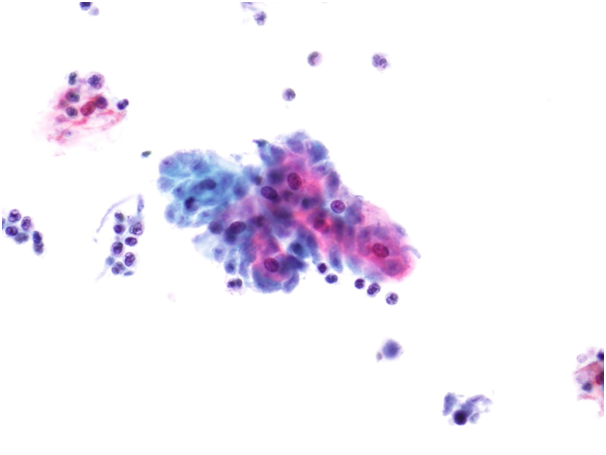
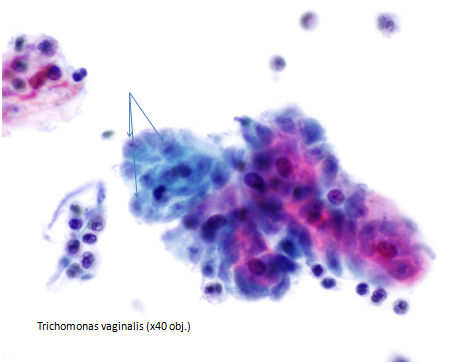
Trichomonal vaginitis is caused by the protozoa Trichomonas vaginalis. It presents clinically with a malodorous and frothy yellow discharge. The protozoa themselves are very small (approx 15 microns) teardrop shaped and very difficult to spot! The cytoplasm often contains eosinophilic granules and the nucleus is centrally located. It is important to diagnose trichomonas as it is a recognised sexually transmitted disease and the womans partner should also be examined.
Trichomoniasis causes local inflammation; the changes are non-specific as described in the section below.
Candidiasis and trichomanaisis do not cause pelvic inflammatory disease.
Immature metaplastic cells and reactive changes due to Trichomonas vaginalis may mimic dyskaryosis if organisms are not seen.
Figure 9b-9 (a-c) Trichomonas vaginalis.
Bacterial Vaginosis is synonymous with the old term Gardnerella vaginalis and includes a variety of anaerobes. The woman may be asymptomatic or present with a white/gray runny and malodorous/fishy discharge. It is a non-inflammatory condition. Clue cells may be present with large numbers of bacteria obscuring the cell borders of squamous cells.
Viral infections
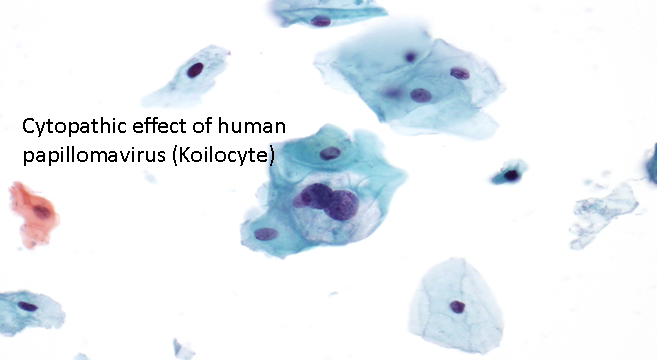
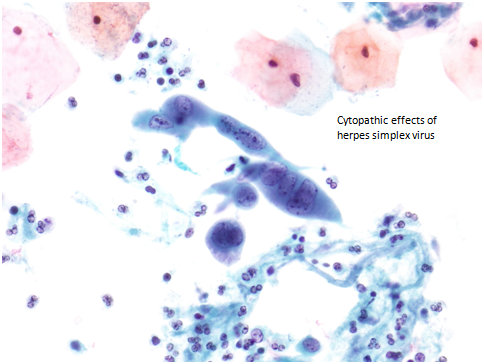
The infecting virus cannot be visualised using a normal light microscope. However two sexually transmitted viruses cause cytopathic effects that we are able to identify in cytology. The first is human papillomavirus and the cytopathic koilocyte, which is considered in chapters on low-grade squamous intraepithelial lesion. The second is herpes simplex.
Herpes virus may be symptomatic and present as blisters; identical to those of the common cold sore, or it can be a dormant infection which is asymptomatic.
It is important to diagnose herpes infection as it may have adverse consequences during pregnancy. Herpes infection is known to cause encephalitis in infants.
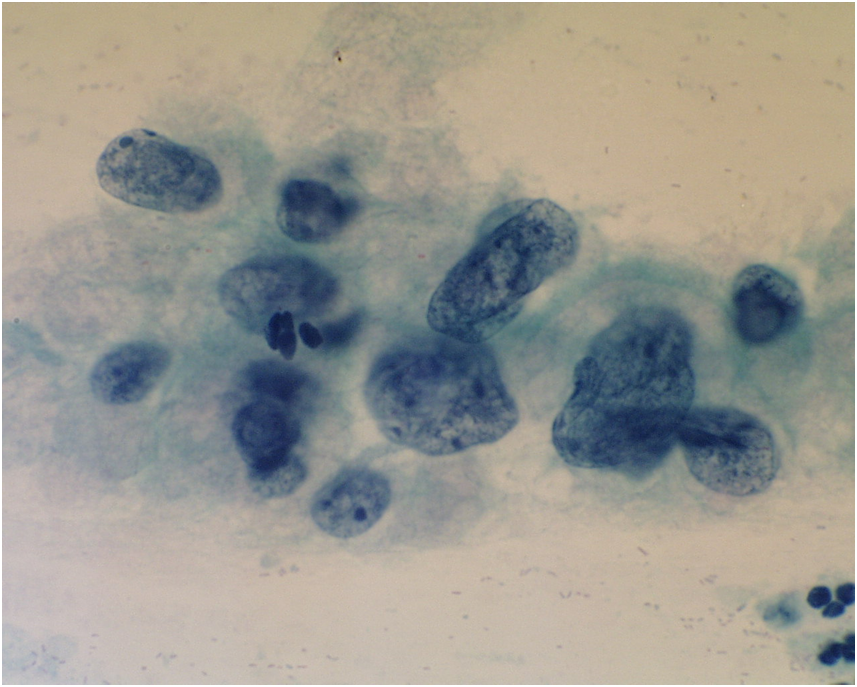
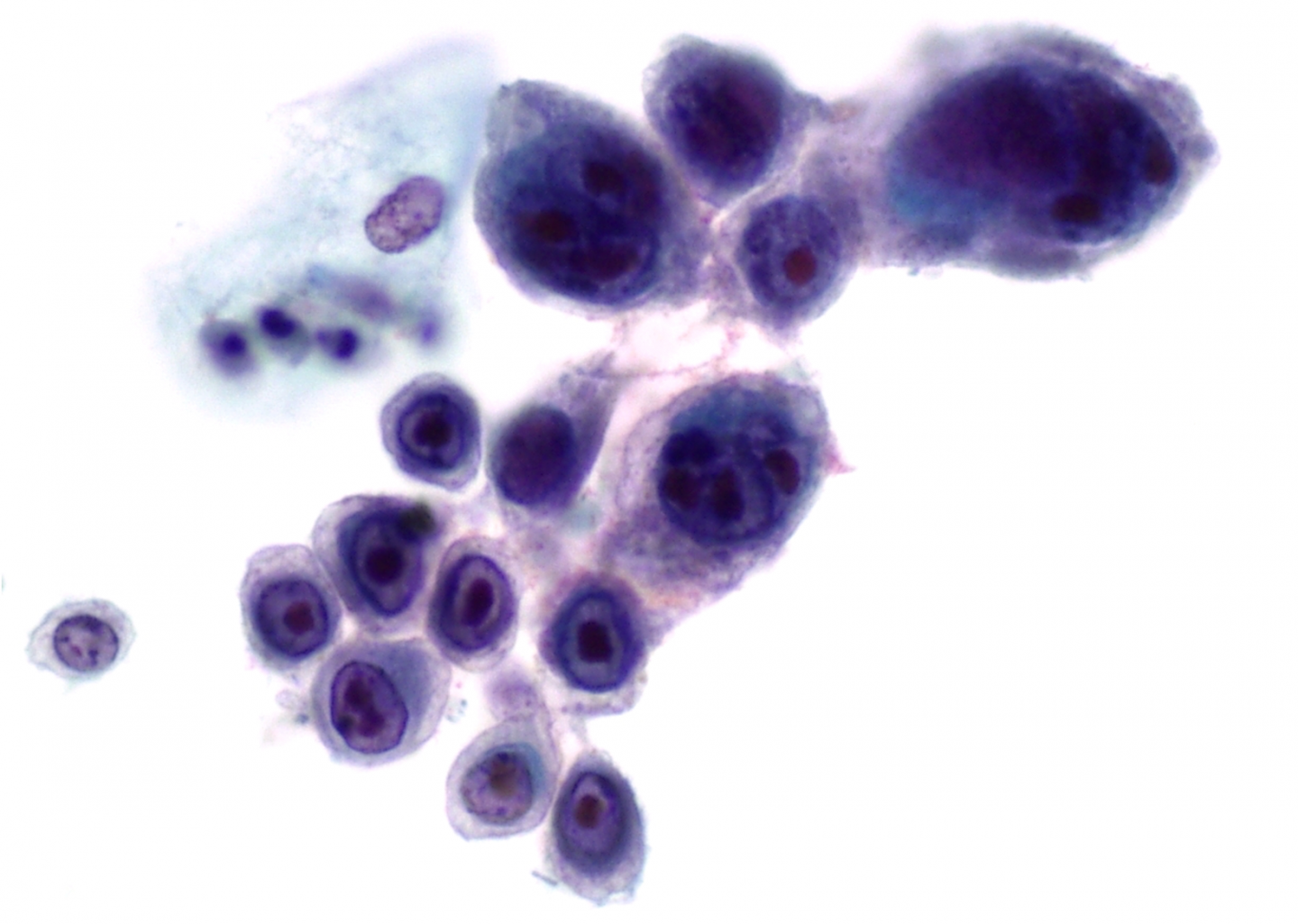
Cytologically, the infected cells display the three Ms of herpes infection
- Margination of chromatin in the nuclei
- Moulding of nuclei
- Multinucleation
Margination of chromatin is caused by the accumulation of viral particles in the nucleus, the chromatin is no longer fine and even, but has a ground glass appearance.
Nuclear moulding is due the fact that the nuclei have outgrown the cytoplasmic area and have to sit closely together. Nuclear inclusions called Cowdry bodies can be seen
Figure 9b-11 (a-b). Herpes virus infection of the cervix (a) Margination of chromatin and ground glass appearance of nuclei (b) Margination of chromatin, multinucleation, cytomegaly and eosinophilic inclusions.
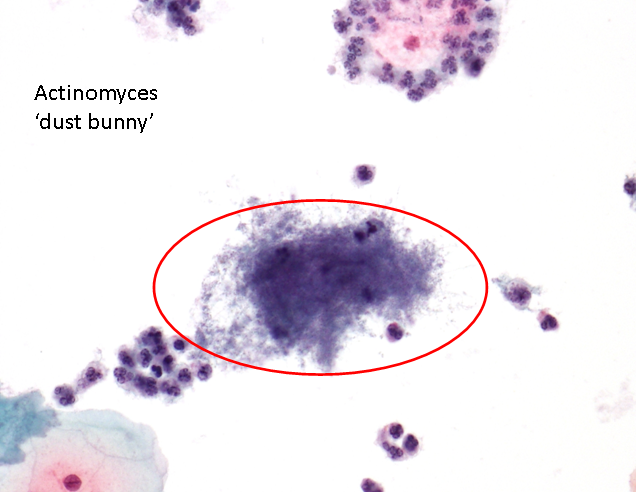
Actinomyces-like organisms
Actinomyces are gram positive, non acid-fact filamentous bacteria that are normally seen in cervical smears of women who have an IUCD.
The bacteria are pseudo-filamentous aggregates that can present in many shapes and sizes. They have a dusty appearance leading to it being colloquially named dust bunny