This content is also available in:
Italiano
Português
Deutsch
Cytological screening has been so successful in preventing invasive cervical carcinoma that its importance as a health problem tends be overshadowed by the disadvantages and possible risks of screening itself.
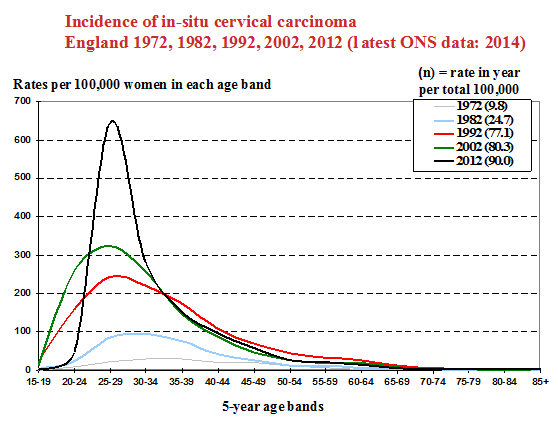
In England, where screening coverage since the NHS Cervical Screening Programme was officially launched in 1988 has been high, CIN3 has most frequently been found and treated in women 25-29 years of age (Figure 5.3). This is also an age group in which reversible HPV infection is commonly found (Figure 5.4) making the distinction between LSIL, a predominantly reversible condition, and HSIL, which carries a risk of progression to invasive cancer, the main focus for cytology.
While symptomatic clinically evident cervical cancer is rare in women under 30 years of age, occult and microinvasive cancers may be found in women aged 25-29 years in well-screened populations (Castanon et al. 2013).
HSIL and LSIL in screened populations
|
Avoiding over-diagnosis of reversible lesions
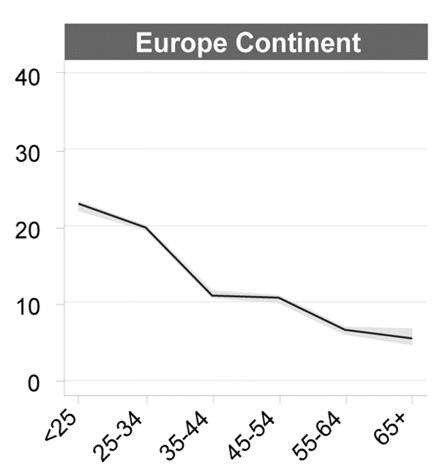
Wilson & Jungner (1968) recognised the potential problem of over-diagnosing borderline lesions (Figure 5.2), which has proved to be a problem with cervical cancer screening. In most laboratories the number of LSIL combined with atypical or borderline cytology reports greatly exceeds that of HSIL. For example, in England (2013-14 data) 1.8% of adequate cytology reports were reported on average as mild dyskaryosis (equivalent to LSIL) or borderline (5.3%) compared with 1.3% high-grade dyskaryosis (equivalent to HSIL) or cancer (HSCIC 2014). Furthermore, rates of HPV-positivity in women with normal cytology in Europe as a whole are even higher (Figure 5.4, from Bruni et al. 2010).
Potentially reversible low-grade and borderline lesions
|

