This content is also available in:
Italiano
Português
Most false negatives are well-recognised types of HSIL, which will not be missed if cytologists are familiar with them.
Small cell dyskaryosis
- Essentially, this is typical carcinoma in situ (CIN3) but the cells may be deceptively small and little larger than neutrophils.
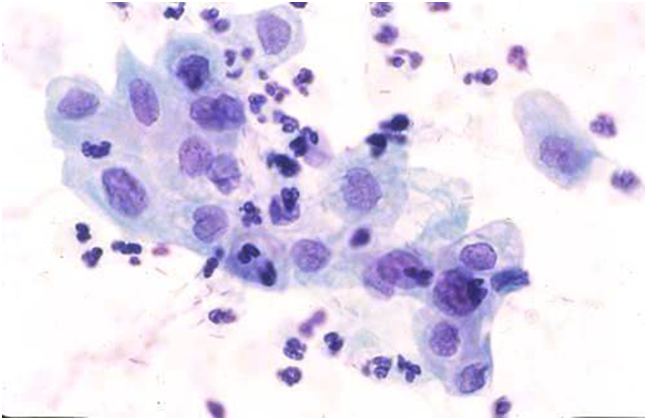
- Attention to the nuclear chromatin pattern will allow this type of HSIL to be recognised even when very few abnormal cells are present as in the single cell below (Figure 10.1 (b), which was the only one on the slide. It was not a false negative and was correctly identified by a diligent screener.


(b) Isolated abnormal cell
Pale dyskaryosis
Although HSIL is usually characterized by hyperchromasia, the nucleus may be pale, making it difficult to distinguish from immature squamous metaplasia or from endocervical cells when the cells are large.
Pale staining may be a feature of regressive Papanicolaou staining
In the BSCC Terminology Conference, approximately one-third of the respondents recognised Figure 10.2 (b) as severe dyskaryosis; one-third diagnosed follicular cervicitis and one-third other reactive change; 4% thought it was glandular neoplasia.
Small and pale cell HSIL as pitfalls in cervical cytology are described and illustrated in detail by Smith & Turnbull (1997).
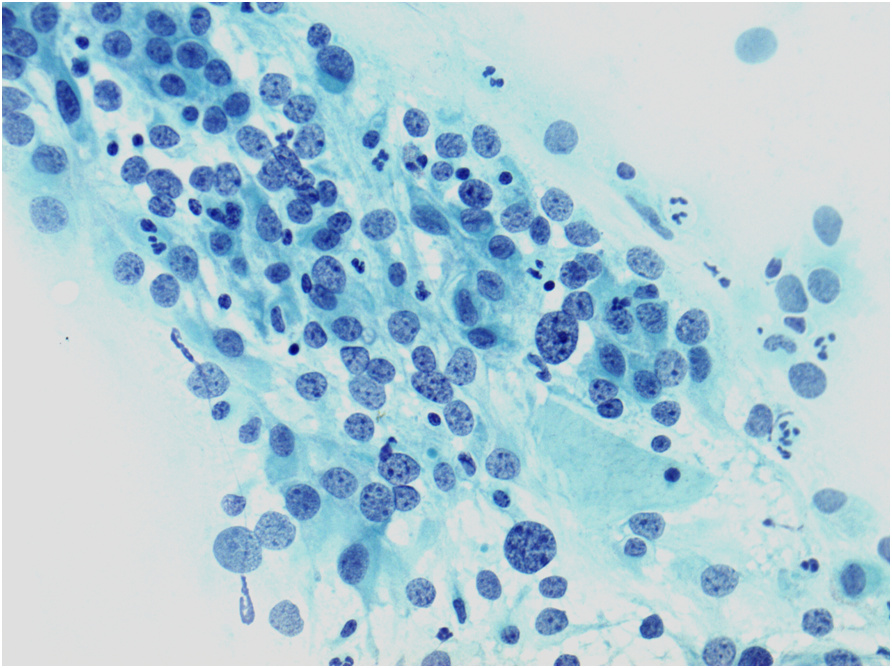
Hyperchromatic crowded cell groups
Microbiopsies or hyperchromatic crowded cell groups of HSIL or even cancer can be overlooked at primary screening or misinterpreted on review. These cells may mimic endometrial cells, sheets of cells from the lower uterine segment or clusters of endocervical cells showing reactive changes.



If the cells are not recognised as HSIL, in these cell groups or elsewhere on the slide, false negatives may be avoided in any or all these cases by reporting them as ASC-H rather than normal or reactive
Inflammatory smears
Misinterpretation of HSIL or even cancer as non-specific inflammation has been a hazard of misdiagnosis in the past. Careful attention to cellular detail on high-power examination should allow this pitfall to be avoided.

Figure 10.4 HSIL+ with severe inflammation
Cytological changes at risk for false negative reports in conventional and LBC slides
- Conventional smears have been shown to be at risk for false negative reports if the cells are small, pale or few in number (Mitchell & Medley 1995; Demay 1996)
- Microbiopsies may be overlooked at primary screening (Robertson & Woodend 1993; Demay 2000). Similar findings have been reported for liquid-based cytology using ThinPrep (Leung et al. 2008).
- Sparse abnormal cells and microbiopsies/hyperchromatic crowded cell groups were found to be the commonest reasons for false negative and potential false negative cytology using SurePath (Gupta et al. 2013).
The main causes of false negative cytology
|
How to avoid false negative results
|

