This content is also available in:
Italiano
Português
While describing the features of the spectrum of squamous and glandular abnormalities seen in cervical cytology and histology it is essential to use terminology that is understood by everyone involved in the screening process and for results to be comparable to those reported in other regions and countries.
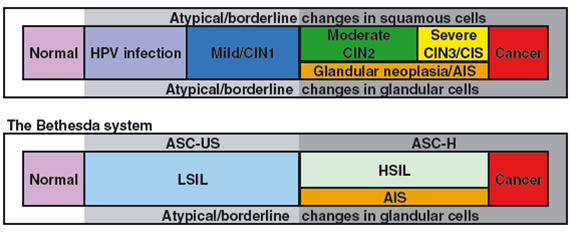
Much of the world uses the Bethesda terminology (Nayar & Solomon 2004), which distinguishes low-grade squamous intraepithelial lesion (LSIL) from high-grade squamous intraepithelial lesion (HSIL) and cancer and describes separate equivocal categories of atypical squamous and glandular cells for instances where a clear distinction between benign and precancerous changes cannot be made.
The European guidelines allow variations in exact terminology (e.g. between dysplasia and dyskaryosis and between atypical and borderline) but their recommendation that all terminology systems should be translatable into the categories used by TBS is the principle used in this chapter. (Herbert et al. 2007; Arbyn et al. 2008). We reproduce here the table comparing TBS with other well-recognised systems used historically for cervical cytology.
Denton et al. (2008) provide a more detailed correlation between TBS and the UK and Australian systems in a publication bringing the UK system closer to TBS.
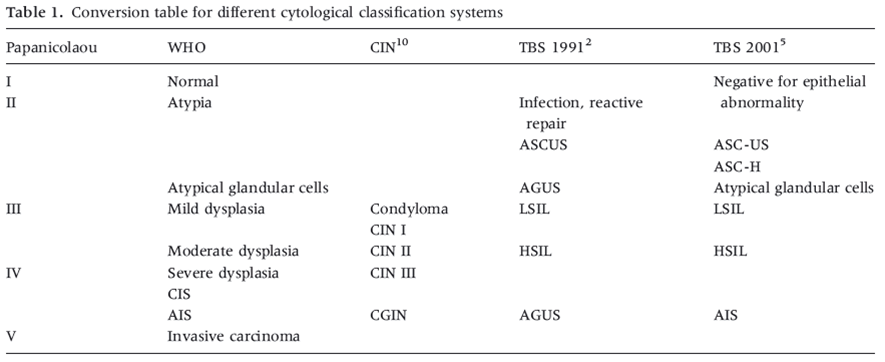
The terminological differences for squamous cell abnormalities are simplified in Table 9a-1 below. Later in the chapter borderline and atypical categories are correlated (figure 9a-4).
Table 9a-1. Correlation of histological categories and the Bethesda and UK systems for cytology terminology
| Histology |
CIN1/HPV |
CIN2 |
CIN3 |
AIS, CGIN or adeno-carcinoma |
SCC |
|
| Histology or cytology |
Mild dysplasia |
Moderate dysplasia |
Severe dysplasia |
CIS |
AIS |
Cancer |
| TBS (cytology) |
LSIL |
HSIL (favour CIN2 or favour CIN3) |
AIS or adeno-carcinoma |
Invasive cancer |
||
| UK system (cytology) |
Low-grade dyskaryosis |
High-grade dyskaryosis (moderate or severe) |
Severe ?glandular neoplasia |
Severe dyskaryosis ?invasive |
||
CIN, cervical intraepithelial neoplasia; AIS, adenocarcinoma in situ; CGIN, cervical glandular intraepithelial neoplasia; SCC, squamous cell carcinoma; CIS, carcinoma in situ, TBS, the Bethesda system; LSIL, low-grade squamous intraepithelial lesion; HSIL, high-grade squamous intraepithelial lesion
Low-grade versus high-grade squamous intraepithelial lesion
- The Bethesda system makes a clear distinction between LSIL, HSIL and cancer rather than using the full spectrum of changes from HPV infection to cancer represented in Figure 9a-2.
- The rationale for simplifying the spectrum as LSIL and HSIL is explained below.
Reversibility of LSIL
Follow-up studies as well as molecular analysis show that LSIL is closely related to reversible HPV infection and is usually (but not always) associated with episomal HPV rather than virus integrated into the host genome. This means that LSIL may logically be managed as a potentially reversible lesion albeit with a risk of progression to HSIL. The BSCC classification agrees with TBS that reversible HPV infection cannot reliably be distinguished from CIN1 and recommends managing them as one entity (Denton et al.)
Risk of progression of HSIL
HSIL, comprising moderate and severe dysplasia/dyskaryosis (correlating with CIN2 and CIN3 on histology) can be regarded as a condition with a sufficiently high risk of invasion to warrant immediate investigation and ablation or excision.
Thus, although the cytological and histological changes are a continuum between CIN1 and CIN3, HSIL should be considered as a relatively infrequent event arising in a background of more frequent and potentially reversible LSIL.
CIN2/moderate dysplasia/dyskaryosis
As the histological and cytological changes are a continuum, moderate dysplasia (CIN2) is an intermediate category, with a greater likelihood of regression than CIN3, which justifies distinguishing it from severe dysplasia but managing it as a condition at risk for progression (Castle et al. 2009; Holowaty et al. 1999).
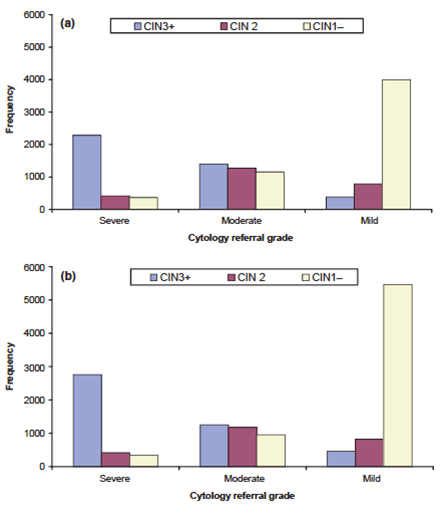
The outcome of moderate and severe dyskaryosis in the English cervical screening programme (with conventional and liquid-based cytology) provides evidence for those preferring to separate HSIL into cases favouring CIN2 and CIN3 respectively and high-grade dyskaryosis into moderate and severe dyskaryosis.