The effects epithelial injury
Injury to the cervical epithelium results in an inflammatory response characterised by localised and systemic changes to the tissue. At the site of injury there is obviously localised damage to the epithelial cells which show degenerative changes to the cytoplasmic and coagulative necrosis of the nuclei.
In the underlying stroma we will see the systemic changes the body uses to remove the insult and repair the injury. There is hyperaemia of the papillary vessels to increase blood flow to the area, exudation of plasma into the surrounding tissue, to bring with it blood products such as fibrin, and a migration of polymorphs to the site of infection or injury.
These changes to the tissue are non-specific and occur regardless of the cause of the injury.
Cytological changes seen with injury
If a cervical smear is taken on an injured cervix we need to consider both cells that are degenerating after the injury, and cells that are regenerating the injured epithelium.
Degenerative changes
The cytoplasm of cells undergoing degenerative changes will show a loss of well defined borders, the cytoplasm is fragile and breaks away leading to a partial or complete loss of cytoplasm, the smear will then contain the remnant bare nuclei. Perinuclear halos are present in most infections together with vacuolation (moth eaten appearance). Ingested polymorphs may be present in the vacuoles.
The nuclei of degenerating cells will initially show swelling or shrinking (due to its inability to control water across the cell membrane) eventually leading to pyknosis. The nucleus has a blurred opaque membrane with clumped chromatin. Eventually and finally there is karyorrhexis (nuclear breakdown) and karyolysis (nuclear dissolution). The inflammatory response will also form a protein rich exudate in which numerous polymorphs will become embedded. Occasionally the polymorphs are so numerous that they obscure the epithelial cells in the smear and render the smear inadequate for evaluation, necrotic cell debris may also be seen in the background.
Regenerative changes
Healing of the ulcerated or eroded epithelium is effected by proliferation of the basal cell layer of adjacent squamous epithelium and expansion of the reserve cells of the local endothelium and crypts. Initially the denuded area is covered by immature metaplastic cells which eventually transforms into mature squamous or columnar epithelium.
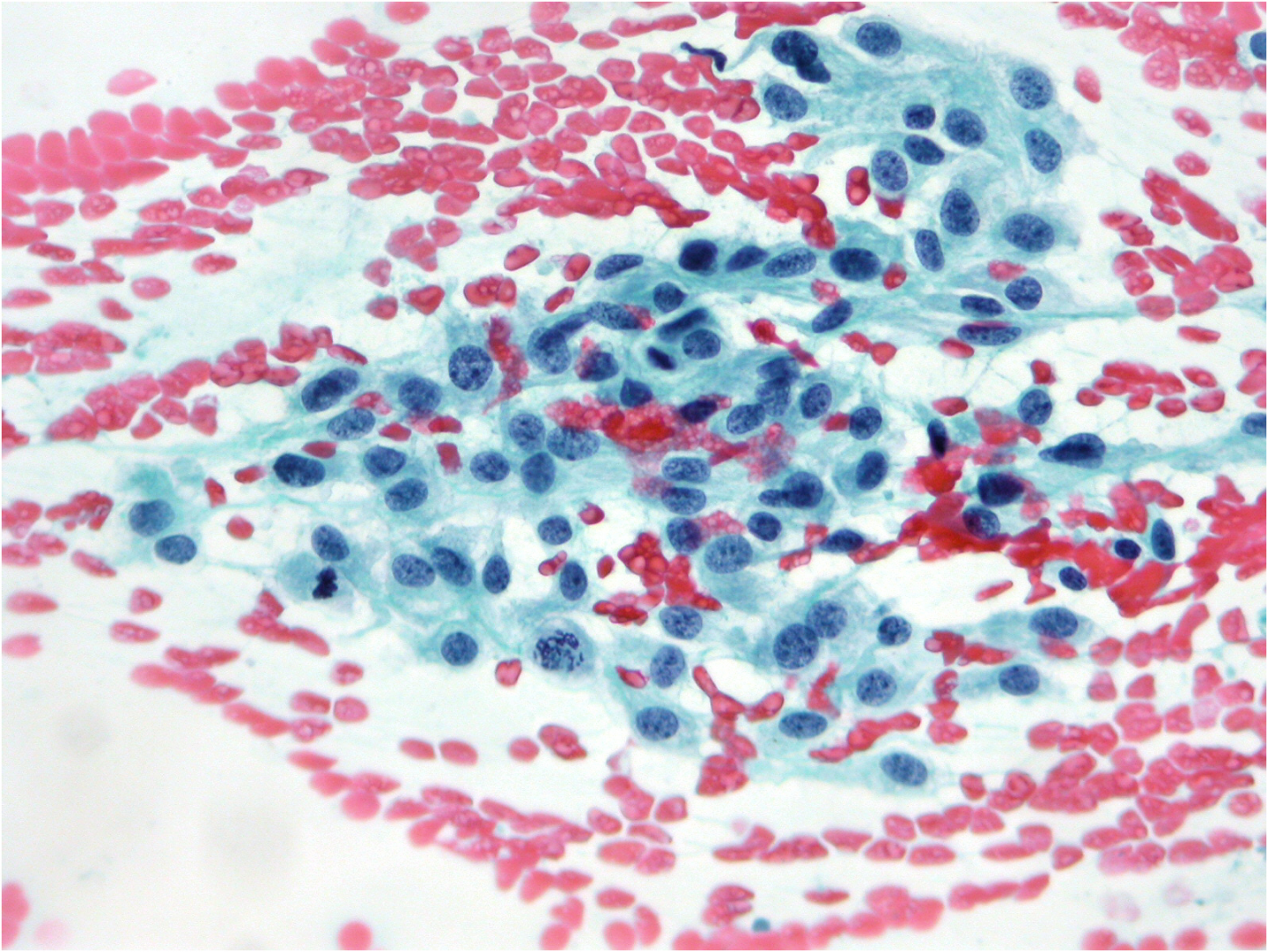
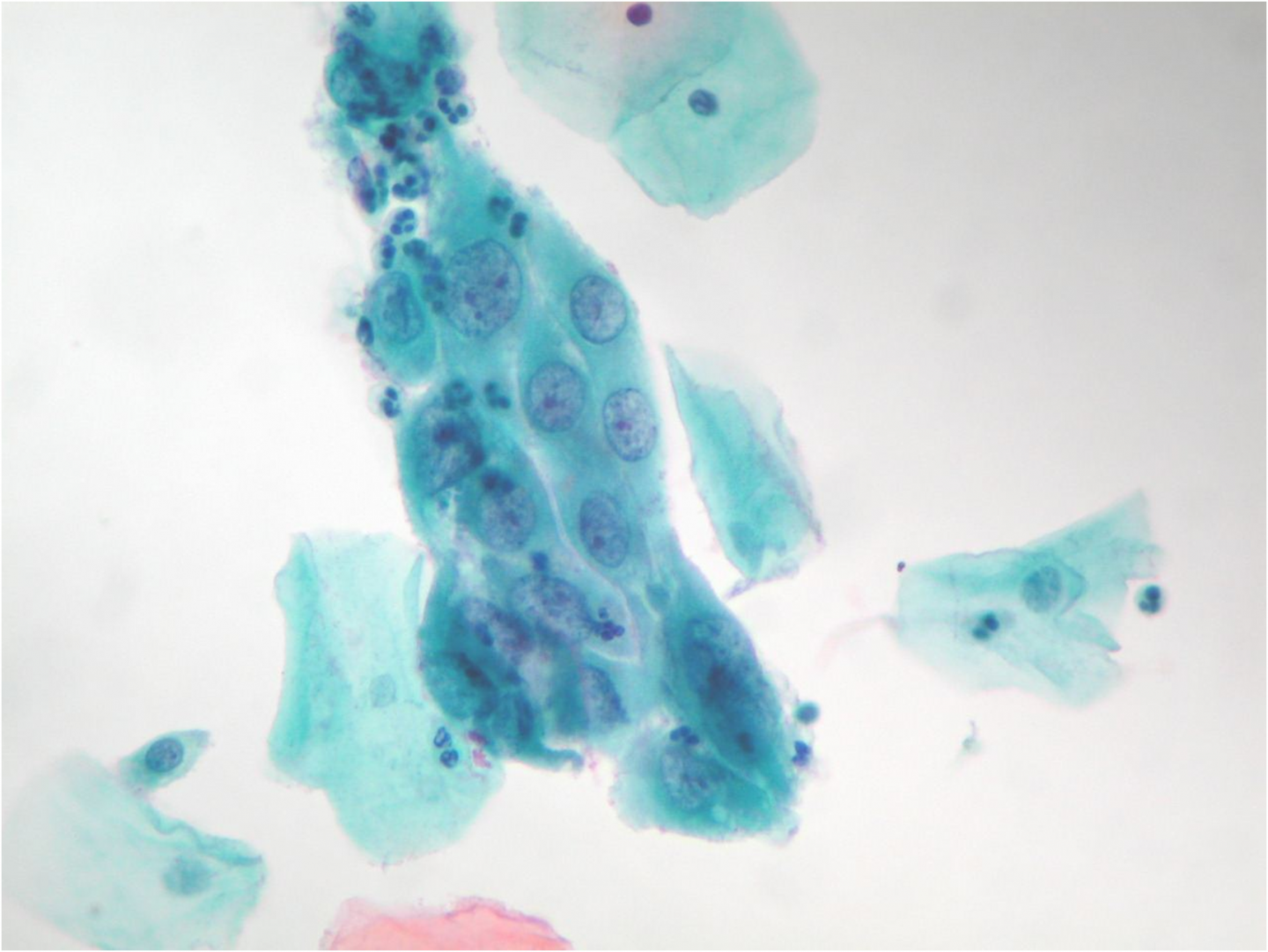
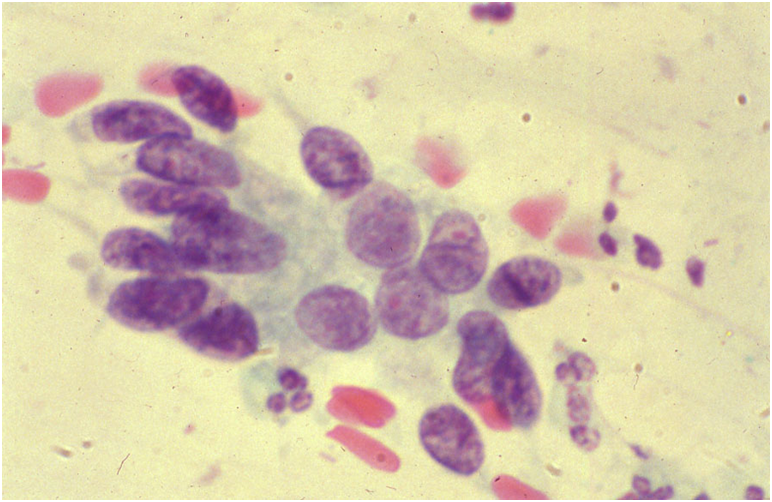
Regenerative changes are characterised by sheets of columnar and immature metaplastic cells with large nuclei and prominent nucleoli or chromocentres reflecting recent mitotic activity. The high-power appearance in LBC is illustrated in Figure 9b-13 (a) below, which is reproduced from Figure 29 from Denton et al. (2008).
When these changes are extreme they may mimic neoplasia representing potential false positive reports.
Figure 9b-13b: Repair change at low power in a conventional smear showing prominent nucleoli and occasional mitoses
Other Inflammatory conditions of the cervix
Atrophic cervicitis
Atrophic cervices are particularly susceptible to infection. An atrophic smear hardly ever has a clear background, it will contain numerous polymorphs and mucus strands and the parabasal cells show degenerative changes such as nuclear pyknosis and karyorrhexis.
Chronic cervicitis
When injury persists, discrete lymphocytes and plasma cells migrate into the inflamed area and can be found in moderate numbers among the polymorphs in the smear. In long standing cervicitis such as that associated with the insertion of a vaginal pessary, for vaginal prolapse, in a post menopausal woman, the epithelium may show reactive changes such as parakeratosis and hyperkeratosis.
Chronic lymphocytic cervicitis is characterised by a mixture of polymorphs and lymphocytes in the smear. Some of the epithelial cells show intense eosinophilic staining consistent with hyperkeratotic changes
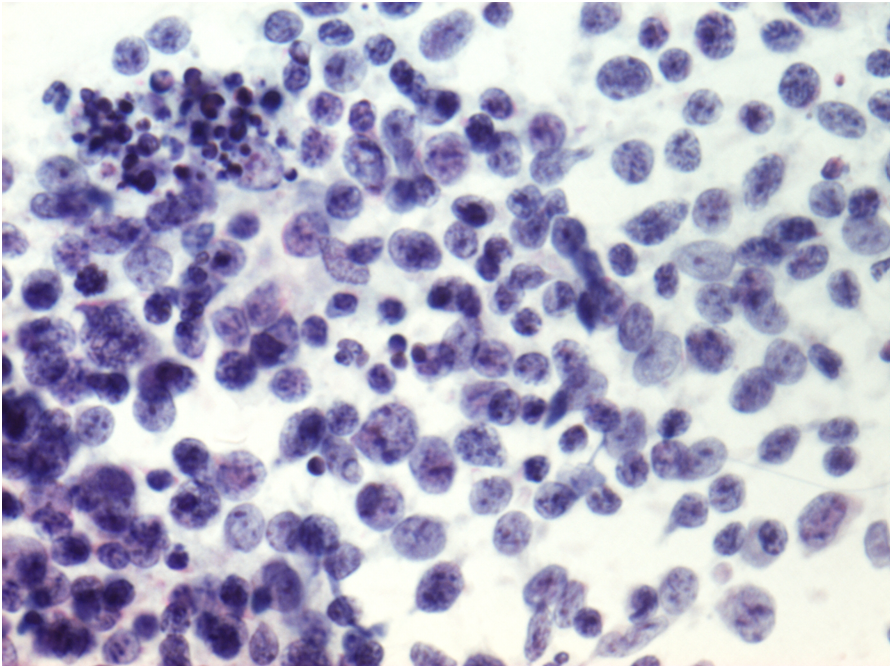
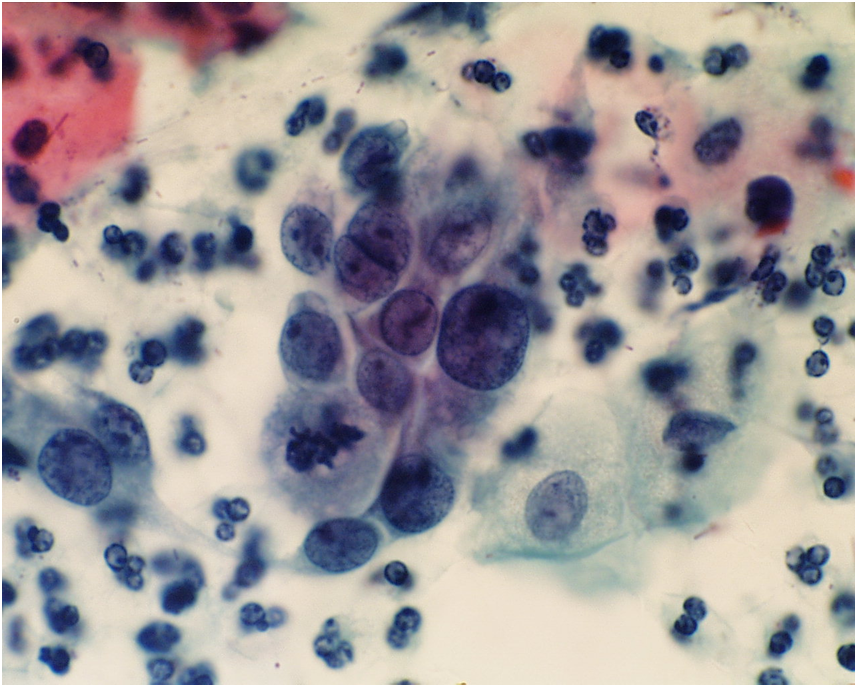
Follicular cervicitis
Follicular cervicitis is a condition characterised by the exposure of lymphoid follicles due to disruption of the overlying epithelium. It can occur at any age but is most common in post-menopausal women whose lymphoid follicles are covered by thin, fragile, atrophic epithelium which is easily removed by the spatula. The smear contains bands of lymphoid cells, both mature and immature, in varying stages of differentiation. Tingible-body macrophages are also present. Marked non-specific inflammatory and repair changes may be seen in the overlying epithelial cells.
Figure 9b-14. Follicular cervicitis: not lymphocytes of variable size and occasional tingible-body macrophages
Non-specific cervicitis and endocervicitis
Non-specific inflammation, endocervicitis, repair and atrophic cervicitis may mimic intraepithelial neoplasia, which is discussed and illustrated in the section on ‘pitfalls’.
| Learning points from Chapter 9bNormal squamous cells, immature metaplastic cells and endocervical cells should be seen on a normal LBC or conventional cervical cytology slide.Endometrial cells, histiocytes, lymphocytes may also be seen and must be distinguished from mature and immature squamous and endocervical cells.Lactobacilli may be seen in normal cervical smears often in those showing cytolysis and bare nuclei.Candida, Trichomomas, Herpesvirus and Actinomyces may be seen in otherwise normal cervical cytology slides.Cytologists must recognise reactive and regenerative changes seen non-specific and specific infections as well as in atrophy and atrophic vaginitis. |