This content is also available in:
Italiano
Português
Deutsch
It is now known that risk factors for cervical cancer are closely related to the persistence of high-risk types of human papillomavirus (HPV) [Walboomers et al. 1999; Li et al. 2011]. Infection by this ubiquitous family of viruses is not the only cause of cervical cancer: its effects must be considered in the context of risk factors that predispose to its persistence and oncongenicity.
Human papillomavirus
HPV is large family of viruses with over 100 types. Studies involving molecular testing of tumour tissue have shown that the great majority of carcinomas of the cervix have integrated viral DNA in the host genome, which is essential to the development of carcinoma.
Prevalence of HPV in cervical cancer worldwideAccording to the meta-analysis by Li et al. 2011 overall prevalence of HPV in human cervical carcinoma was between 85.9% and 92.9% depending on the date of publication of the analysis |
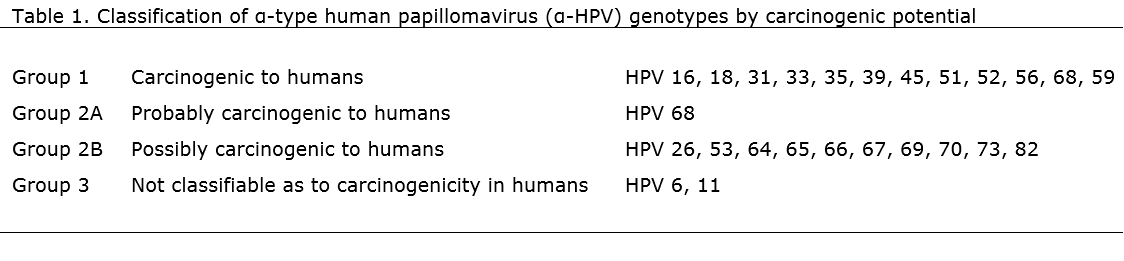
The anogenital types of HPV involved in cervical cancer and genital warts are members of the ?-genus of HPV and are categorized as two main types: high-risk and low-risk (Table 3.4, Cubie & Cuschieri 2013).
Clinical associations of high- and low-risk HPV
Low-risk HPV is associated with condylomas (genital warts) and is most likely to be a transient infection. In most cases, the immune system is able to fight off the infection through apoptosis of infected cells and repair any damaged tissue through the regeneration of new squamous epithelium.
High-risk HPV is similar in that infection is usually transitory, but it has a greater likelihood of persistence. Coupled with other risk factors, high-risk HPV is able to integrate into the host DNA and, over time and if left untreated, has the potential to develop into carcinoma.
High-risk HPV in cervical carcinomas in EuropeBased on a retrospective cross-sectional study by
de Sanjose et al. 2010
HPV 16 – 66%
HPV 18 – 7%
HPV 33 – 6%
HPV 45 – 4%
HPV 31 3%
Types 16, 18 and 45 commonest in adenocarcinoma
|
High-risk HPV in head and neck cancers
High-risk HPV has also been shown to be a causal agent in oropharyngeal carcinoma (Gillison et al. 2000; Chaturvedi et al. 2011).
Other risk factors for cervical cancer
Cervical cancer incidence depends on prevalence of high-risk HPV in the population along with other co-factors, such as sexual activity and pregnancy from an early age, cigarette smoking, immune competence, type and duration of contraceptive use, diet and socio-economic status (Gadducci et al. 2011; International Collaboration of Epidemiological Studies of Cervical Cancer 2006). Diet may also have a role, as may the use of barrier contraception (Piyathlake et al. 2004; Hogewoning et al. 2003).
Prevalence of these risk factors may change in different birth cohorts, which has to be taken into account when assessing incidence and mortality with respect to the effect of both opportunistic and organised screening (Bray et al. 2005).
Risk factors other than HPV (some are related to HPV exposure) that have been reported for developing cervical carcinoma are:
- Cigarette smoking
- Immunosuppression
- Chlamydia infection
- Poor diet
- Obesity
- Number of sexual partners
- Sexual activity from an early age
- Long-term use of oral contraceptives
- Long-term use of intra-uterine device
- Multiple full-term pregnancies
- Giving birth younger than 17 years of age
- Poverty
- Family history
Predisposition to these risk factors other than high-risk HPV indicates a higher susceptibility, not an assurance, for developing cervical cancer.

