The section above describes how to recognise the main presentations of HSIL. ASC-H should be rare if cytologists concentrate on the abnormal chromatin pattern and irregular nuclear membranes seen in HSIL and are aware that
- HSIL may have relatively small and pale nuclei
- Hyperchromatic crowded groups of cells may have recognisable HSIL cells at their periphery or between the cell groups
- Diagnoses can usually be made on sparse abnormal cells and
- Cases on the borderline between HSIL and LSIL should be defined as SIL and not ASC-H.
In most countries ASC-H is not subjected to HPV triage so the diagnosis depends on colposcopy appearances and accurate biopsies. In the UK all borderline diagnoses, including ‘cannot exclude high-grade dyskaryosis’ are subjected to HPV triage and only investigated if positive. It is there important not to miss the occasional HSIL that is HPV-negative.
In practice there are three main situations in which the ASC-H category is used
- Sparse dyskaryotic cells
- Hyperchromatic crowded cell groups
- Distinction between immature squamous metaplasia and HSIL
In the first instance avoided ASC-H may be avoided by consultation with colleagues and confidence in recognising HSIL.
In the second group ASC-US can again be avoided by consultation and recognition of the main look-alikes of hyperchromatic crowded cell groups: endometrial cells, tubo-endometrioid metaplasia, reactive endocervical cells and CGIN. Concentration on cells dissociating from the main cell group and situated between those groups usually allows the diagnosis to be made when HSIL is present. As hyperchromatic crowded cell groups more often represent CIN3 than CIN2 the nuclear atypia and NC ratio should be diagnostic in HSIL.
The third group probably causes the most difficulty because there may be a genuine difficulty in distinguishing immature squamous metaplasia, and sometimes tubal metaplasia, from the ‘metaplastic’ type of HSIL.
Immature squamous metaplasia versus HSIL
The distinction of HSIL from immature squamous metaplasia may be equally difficult in histological sections resulting in the concept of ‘immature squamous metaplasia’, which probably represents LSIL in immature metaplasia (Duggan et al. 2006). High-grade HPV triage can help distinguish SIL from immature metaplasia; p16 and Ki-67 may be useful in distinguishing HSIL from LSIL in this context. In cytology, the main distinction is between HSIL and immature squamous metaplasia and depends on the chromatin pattern, nuclear membrane irregularity and NC ratio as described above.
Examples given in Figure 9c-16, 17 and 18 would justify a diagnosis of ASC-H.
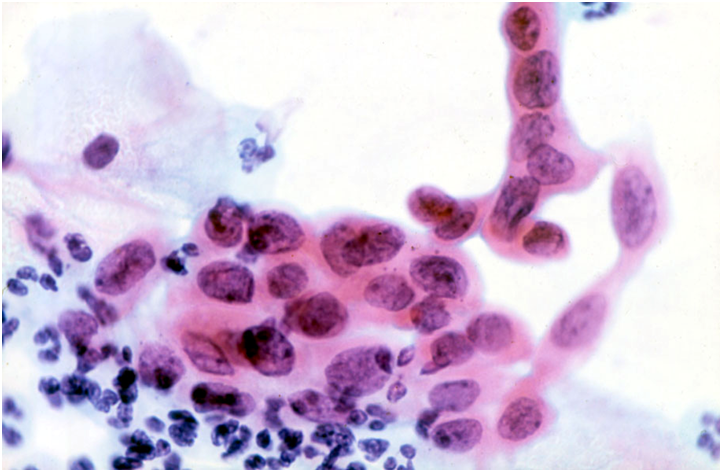
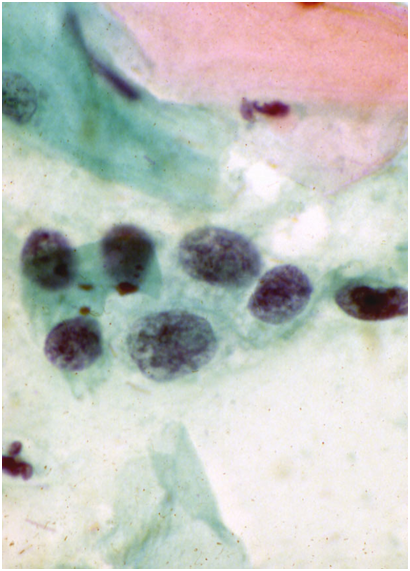
Figure 9c-16 (a-b). ASC-H in immature metaplastic cells
(a) ASC-US confirmed as CIN2 on biopsy
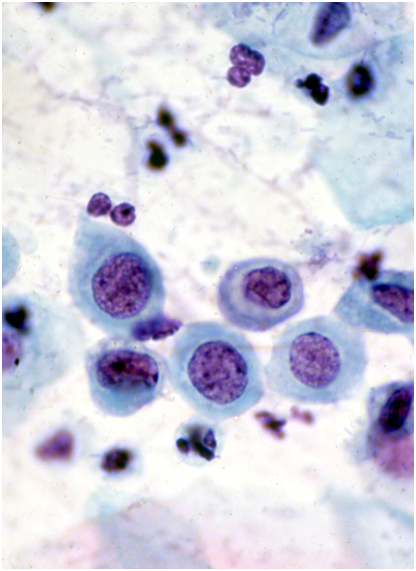
Figure 9c-17 (a-b). ASC-H in sparse atypical cells.
(a) ASC-H confirmed as CIN2
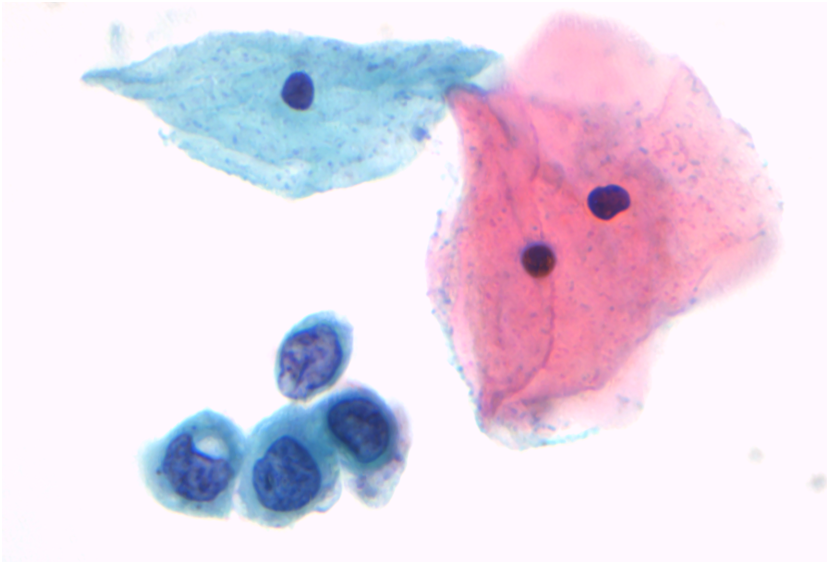
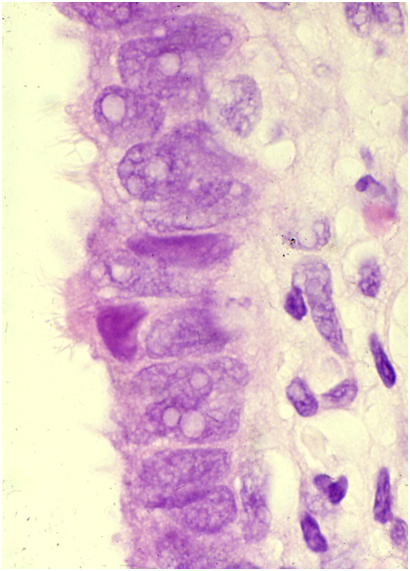
Figure 9c-18 (a-b). ASC-H in tubal metaplasia.
(a) Shows the typical round nuclei of tubal metaplasia: one basal plate can be seen but no recognisable cilia.