This content is also available in:
Italiano
Português
Deutsch
Čeština
Română
Türkçe
CIN and squamous cell cervical carcinoma
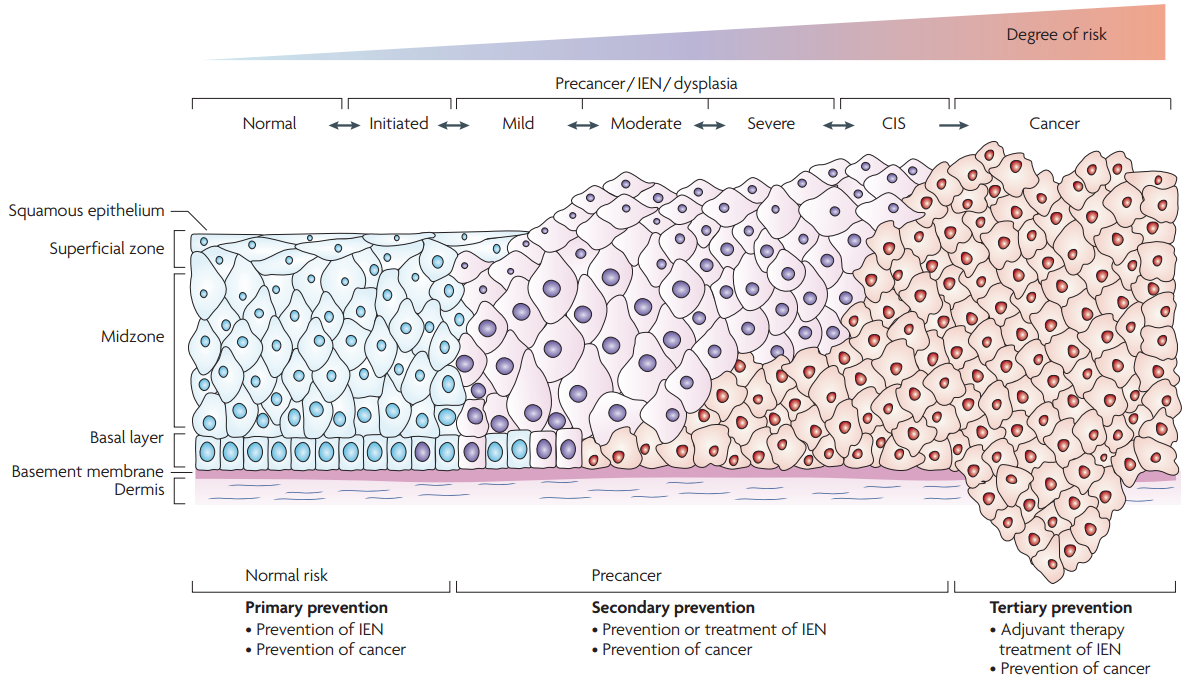
It is widely accepted that invasive squamous cell carcinoma of the cervix, which is the commonest histological type, is preceded by a pre-invasive stage of the disease, where the abnormal cells are confined to the epithelium. This stage of non-invasive disease is known as cervical intraepithelial neoplasia (CIN) and is directly related to the processes of infection and integration of HPV as described in the previous chapter. [Link to Chapter 3 Epidemiology and aetiology]
The development of CIN involves a progression from early changes (CIN1) involving the deeper layers of the epithelium to full thickness involvement at its most severe (CIN3) equating to carcinoma in situ (Figure 4.1).
|
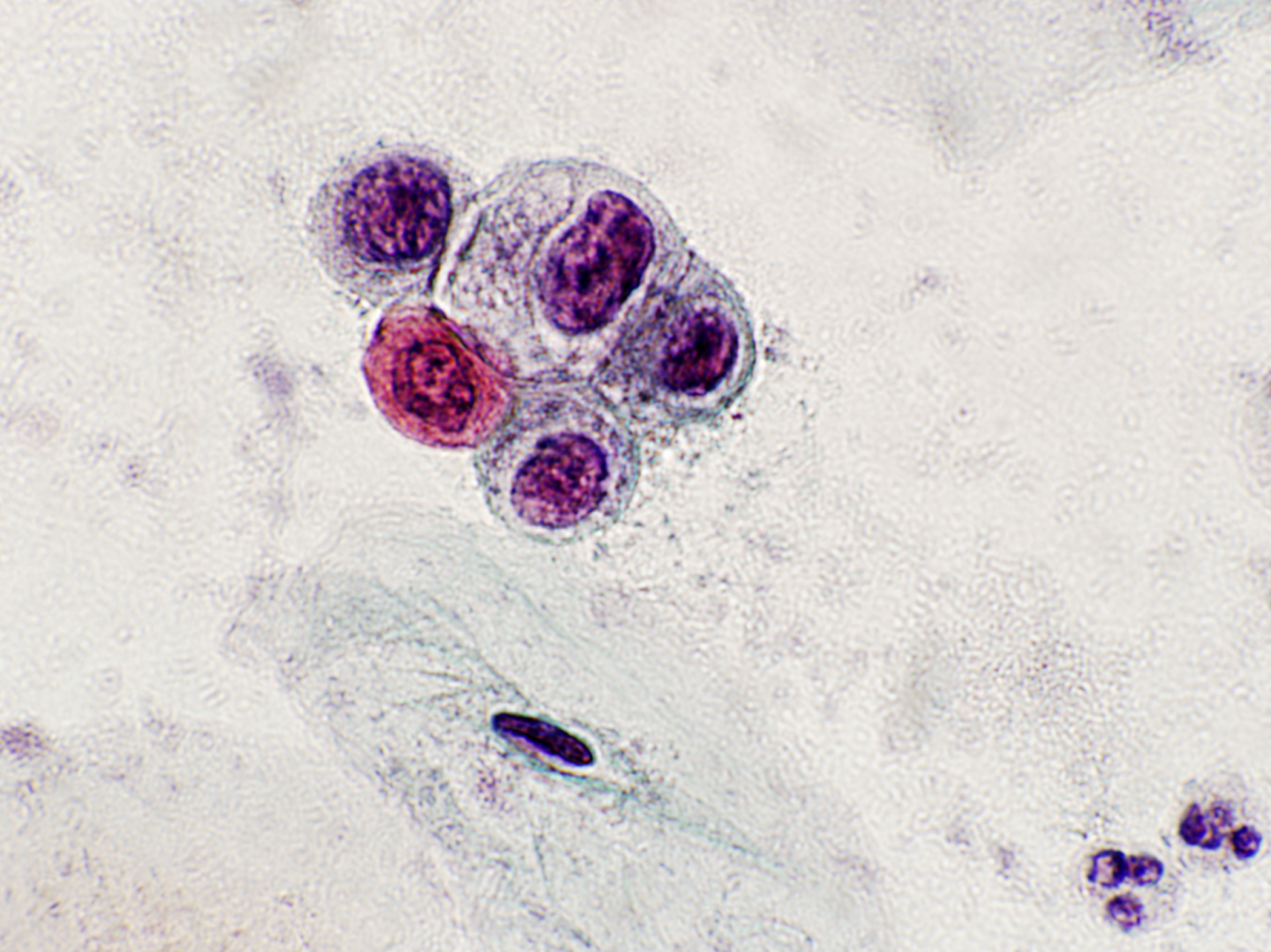
Figure 4.2 (a-c). CIN1
FIGURE
(a) CIN1 in a cervical biopsy; (b) LSIL in a Pap smear; (c) LSIL with koilocytosis (see Figures 9c-2a and 9c-3b in Chapter 9c and scanned slides linked to that chapter).
CIN1 overlaps with HPV infection and usually resolves spontaneously within 9-12 months. There are numerous follow-up studies of CIN1 showing a highly variable risk of progression to CIN2-3 and a consequent risk of invasive cancer in a small minority of patients (Ostör 1993; Holowaty 1999; Bansal et al. 2008).
A large retrospective follow-up study of mild, moderate and severe dysplasia by Holowaty et al. showed that the majority of cases of mild (62.2%) and moderate dysplasia (53.7%) regressed (two negative smears within 2 years) while progression to moderate dysplasia or worse was approximately 25% within 5 years, which is consistent with other studies.
Progression of mild dysplasia (from Holowaty et al.)Moderate Severe+ Within 2 years 11.1% 2.1% Within 5 years 20.4% 5.5% Within 10 years 28.8% 9.9% |
Likelihood of progression depends on persistence of HPV, its integration into the host genome and its type (Jaisamrarn et al. 2013).
- HPV16 and 33 have the highest risk of progression to CIN3
- HPV16 and 31 to have the least likelihood of regression
High-grade CIN
CIN2 and CIN3 are managed as high-grade CIN and usually treated by excision or ablation when diagnosed at colposcopy.
CIN2 is an intermediate lesion and there is evidence from the ALTS trial that around 40% resolves spontaneously but was less likely to do so when HPV16-related (Castle et al. 2009). The retrospective study by Holowaty et al. (1999) showed that the majority of moderate dysplasia regressed dysplasia regressed (53.7%) while progression was more likely than for mild dysplasia.
Progression of moderate dysplasia (from Holowaty et al.)Severe+ Within 2 years 16.3% Within 5 years 25.1% Within 10 years 32.0% |
The cumulative actuarial rate of progression at 5 years per 100 women of moderate dysplasia (1.2) to invasive cancer was intermediate between mild (0.4) and severe dysplasia (3.9). (See Holowaty et al. 1999 for complete data with confidence intervals.)
CIN2 is defined by nuclear pleomorphism with mitotic activity extending to the upper two-thirds of the epithelium. There is usually little or no koilocytosis.
Figure 4.3 (a-b). CIN2 (moderate dysplasia): intermediate risk of progression
FIGURE
(a) HSIL, favour CIN2, on a LLETZ; (b) HSIL (favour CIN2) (see Figure 9c-7b and scanned slides linked to Chapter 9c)
In view of its intermediate position between CIN1 and CIN3 in terms of risk of progression and the clinical importance of deciding whether CIN2 should be managed as a high-grade precancerous lesion, immunohistochemistry using the cyclin-dependent kinase inhibitor p16INK4A is now recommended in the US to improve consistency of diagnosis and define high-grade CIN (Galgano et al. 2010; Darragh et al. 2012).
P16INK4A staining helps distinguish CIN2 from
|
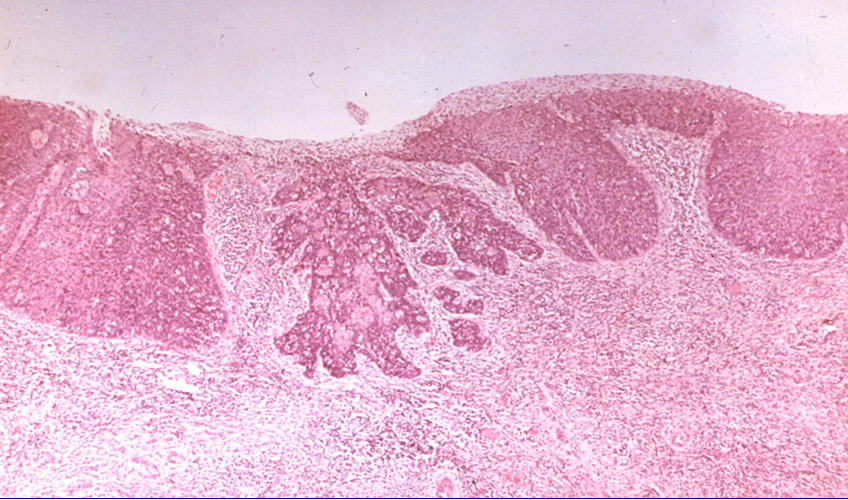
CIN3 is defined by nuclear pleomorphism involving the full thickness of the squamous epithelium with mitotic activity at all levels. CIN3 (and severe dysplasia) equates to carcinoma in situ, which term is seldom used nowadays.
Risk of progression is highest for CIN3 and inter-observer variation is considerably less than for CIN1 or CIN2 (Stoler et al. 2001). Microinvasive carcinoma is almost always seen in a background of widespread CIN3 further demonstrating its malignant potential. The exact risk is difficult to calculate because most CIN3/carcinoma in situ is treated when diagnosed.
Figure 4.4 (a-c). CIN3 and occult cancer