This content is also available in:
Italiano
Português
Deutsch
Adenocarcinoma
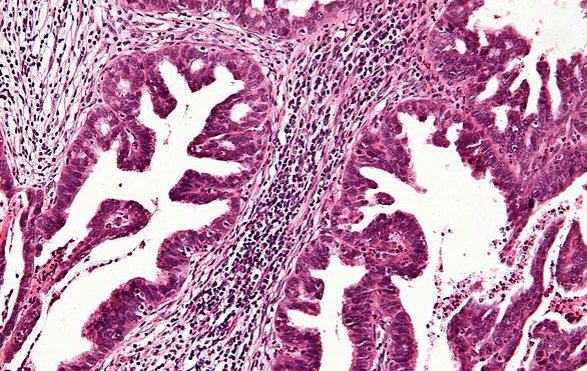
Adenocarcinoma of the cervix is a malignant neoplasm that involves the glandular epithelium of the cervix. There are several types of adenocarcinoma, most of which have similar aetiology and risk factors to squamous cell carcinoma. Endocervical-type mucinous adenocarcinomas comprise 70% of adenocarcinomas (WHO).
HPV types commonly associated with adenocarcinoma are 16, 18 and 45 (de Sanjose et al. 2010).
Adenocarcinoma is more difficult to prevent than squamous cell carcinoma and is therefore more frequent in well-screened populations (Bulk et al. 2005). While WHO quotes 10-15% of cervical cancers to be adenocarcinoma (WHO), a national audit in England showed 19% of 3,305 carcinomas of known type to be adenocarcinoma and 4% to be adenosquamous carcinoma (Sasieni et al. 2009).
Studies in Europe, the UK and elsewhere (Sasieni et al. 2009; Bray et al. 2005; Viczaino et al. 1998) consistently support the statements below.
|
Adenocarcinoma in situ (AIS)
Endocervical-type adenocarcinoma is the commonest (70% of adenocarcinomas) and may be preceded by adenocarcinoma in situ (AIS), also known as cervical glandular intraepithelial neoplasia (CGIN), which is a known precursor of adenocarcinoma (Ostör et al. 2000).
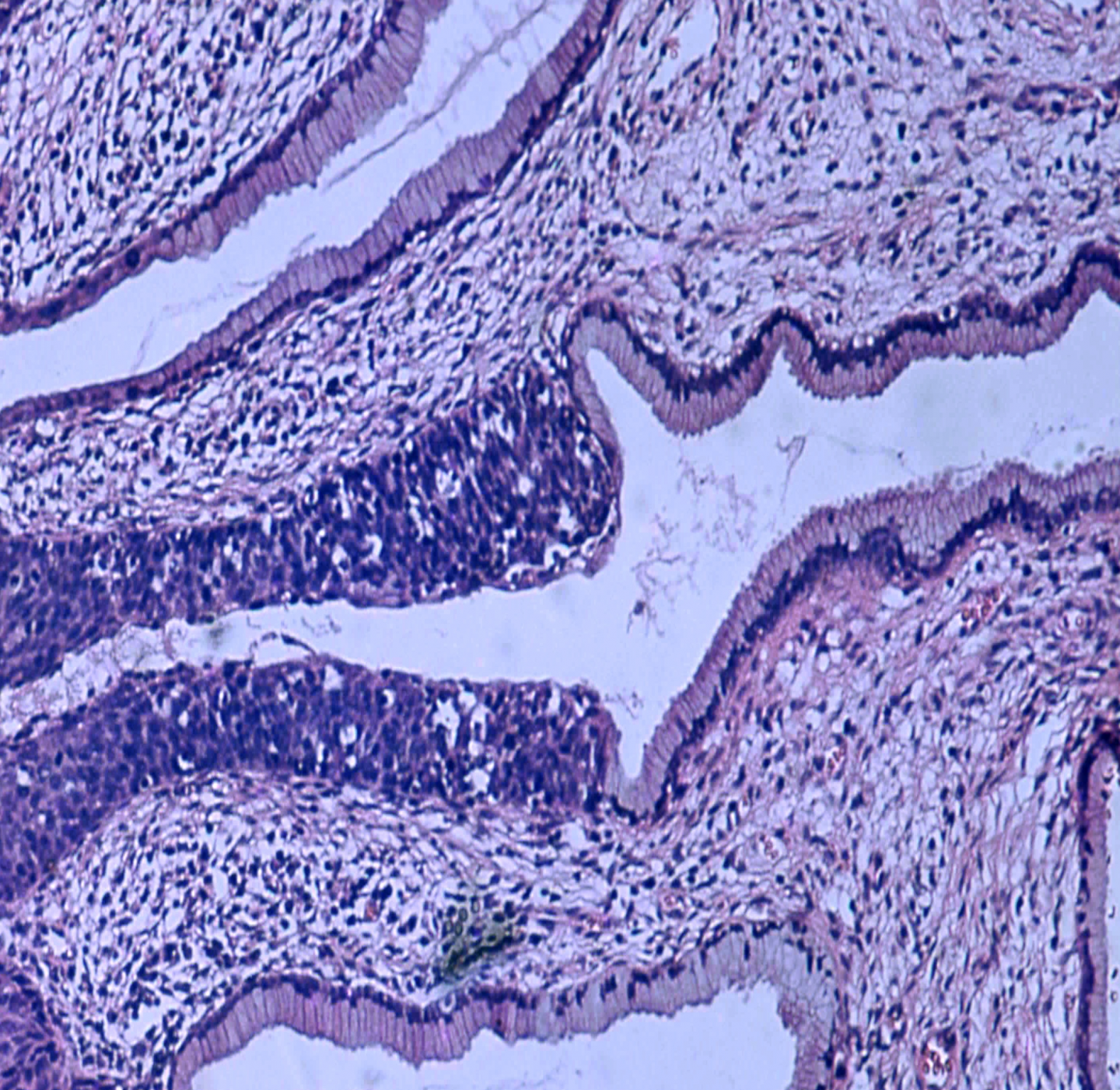
Although low-grade and high-grade CGIN has been described it is usually regarded as a single entity and managed as AIS. CGIN often coexists with high-grade squamous CIN, which may make it easier to detect on cytology and at colposcopy (Talaat et al. 2012). Colposcopy is less sensitive in detecting glandular abnormalities compared with squamous cell lesions (Jordan et al. 2008; Talaat et al. 2012).
Woodman et al. (2003) suggest that HPV18 pre-invasive lesions may be less likely to present as high-grade abnormalities thus compromising their detection on cytology.
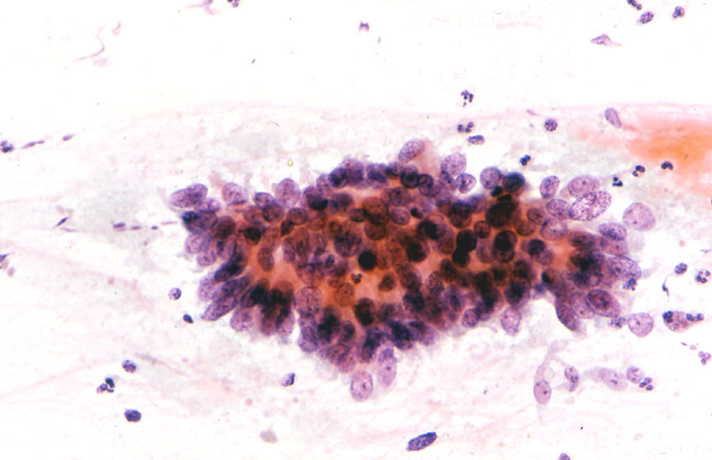
Cytological diagnosis of adenocarcinoma and AIS
Cytology is important in detecting occult adenocarcinomas as well as AIS: 15% of adenocarcinomas have no visible lesion (WHO). A national audit in Sweden reported 65% of 186 adenocarcinomas as screen-detected (following abnormal cytology within 6 months) compared with 33% of 615 squamous cell carcinomas (Andrea et al. 2012).
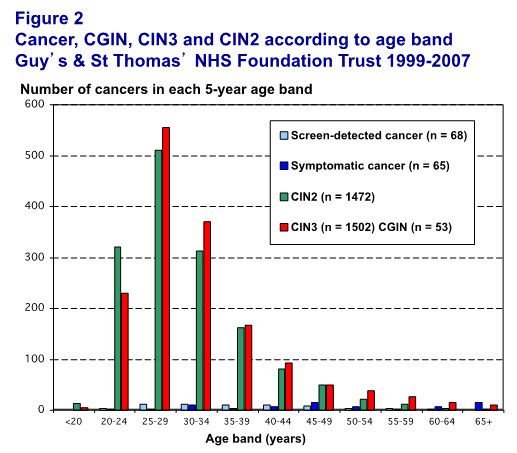
AIS/CGIN is less frequently detected than CIN3 as shown in Figure 4.6 below. In that audit of 133 cancers, 113 were squamous cell carcinomas, 14 adenocarcinoma (half were screen-detected), four adenosquamous and two other types indicating a lower ratio of in situ to invasive adenocarcinoma (4:1) compared with squamous cell carcinomas (13:1) (Herbert et al. 2010).
Adenocarcinoma in situ (CGIN) summary
|

