In the majority of cases, an experienced cytotechnologist or pathologist can make the distinction between benign epithelial cells and neoplastic cells with a high degree of confidence. However, in what should be a small proportion of cases, there may be genuine doubt as to whether the epithelial cells are benign or neoplastic.
In TBS these changes are described as ‘atypical squamous cells’ and in the UK system ‘borderline changes in squamous cells’. Most ASC is on the borderline between normality and LSIL and is referred to as ‘atypical squamous cells of undetermined significance (ASC-US). A minority of cases there is uncertainty between benign/reactive changes and HSIL or cancer: atypical squamous cells cannot exclude HSIL (ASC-H) will be considered later in this chapter.
There are two main situations in which the ASC-US category may apply:
- Changes such as double nuclei, parakeratosis and minimal nuclear changes suggesting HPV effect but without definitive koilocytosis.
- Samples in which it is genuinely difficult to distinguish benign, reactive or degenerative change from LSIL.
There are several features that must be present to use the ASC-US report.
- Squamous differentiation
- Some form of chromatin irregularity in the form of mild hyperchromasia/granular or smudged chromatin/multinucleation etc.)
- Nuclear enlargement more than twice the size of the equivalent normal cell (TBS definition). The degree of nuclear enlargement has been shown to be similar to LSIL (Slater et al., 2005a)
- Slightly increased nuclear/cytoplasmic (NC) ratio
ASC-US in which HPV is suggested but koilocytosis is not present
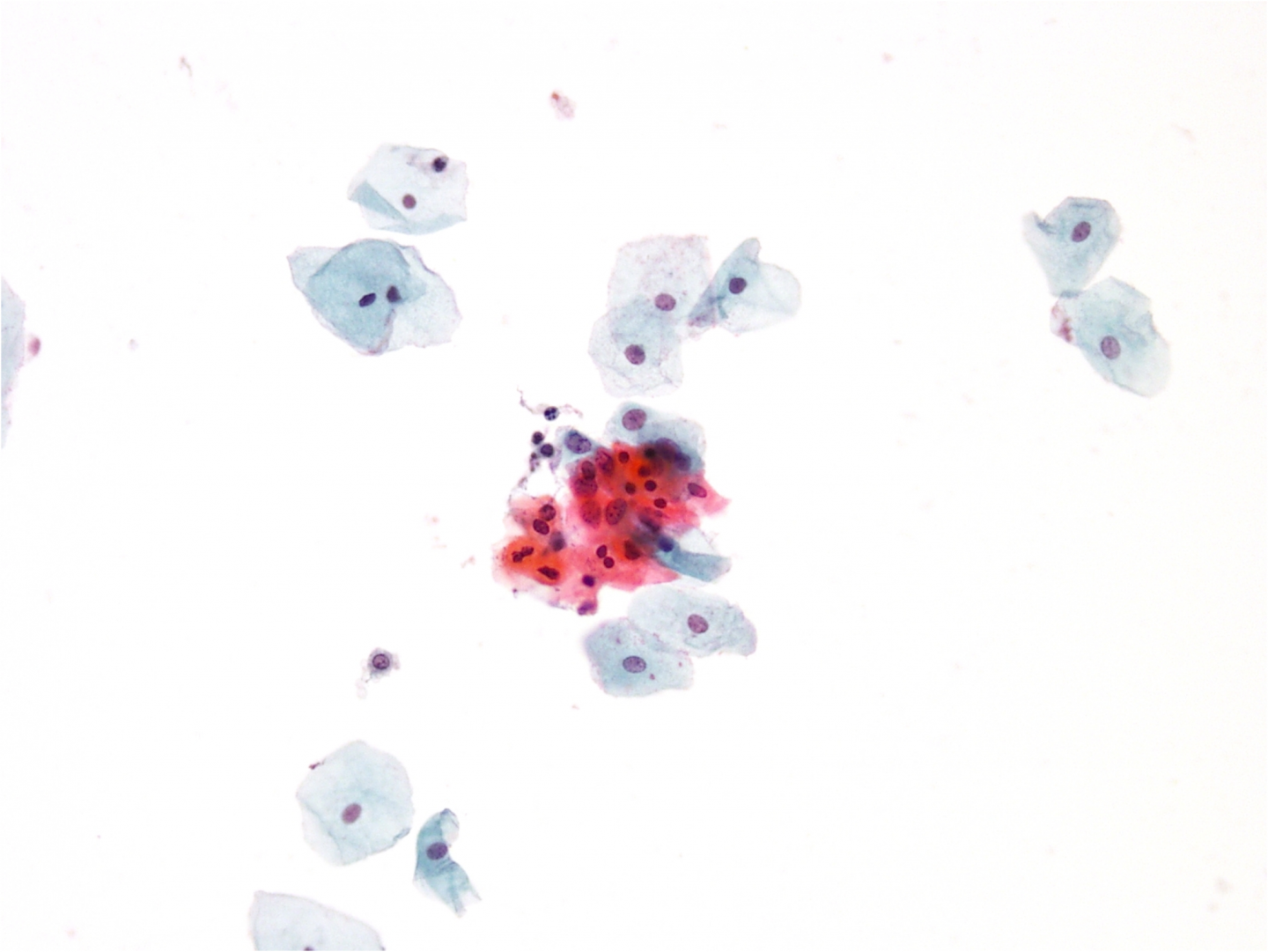
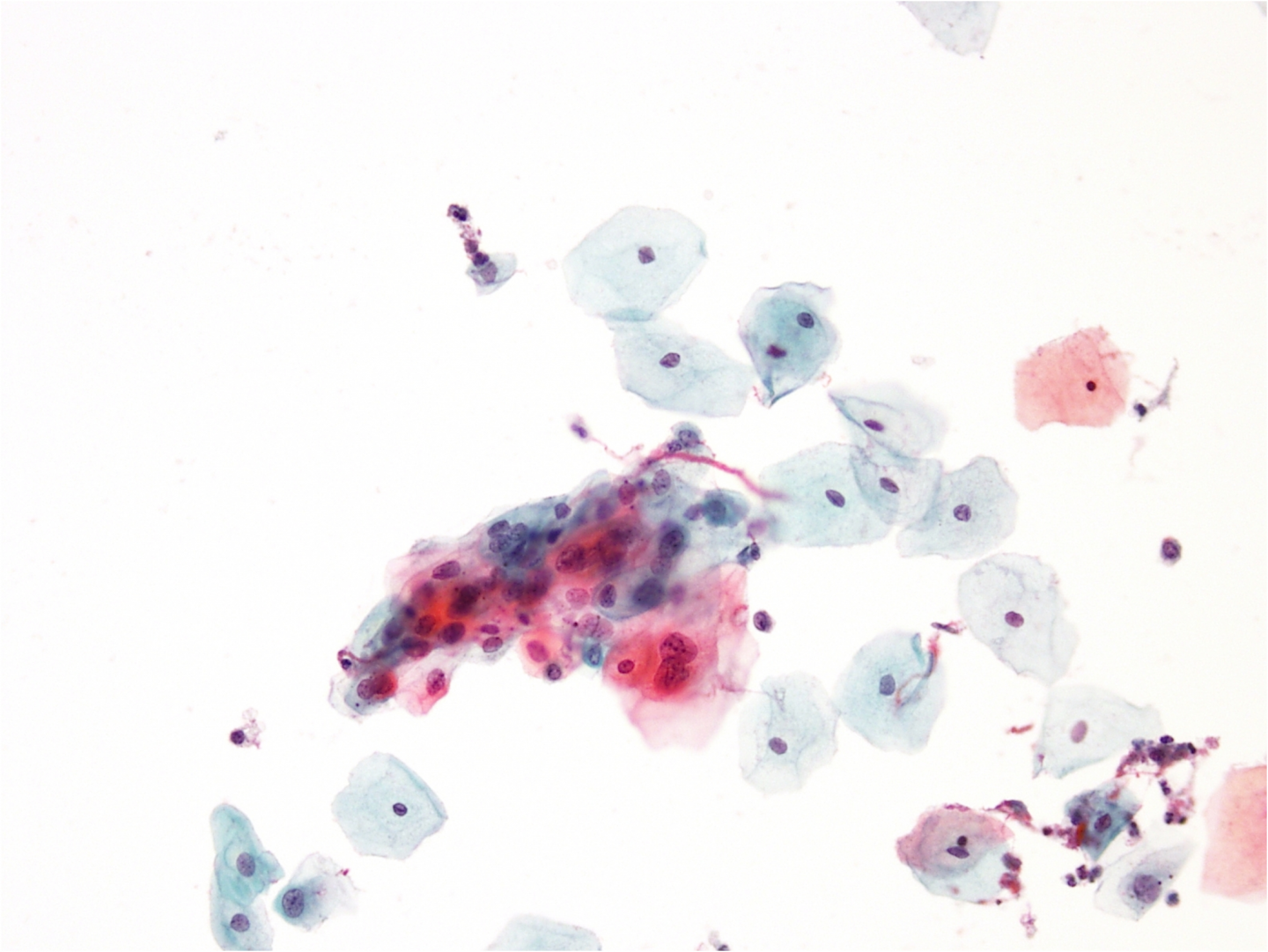
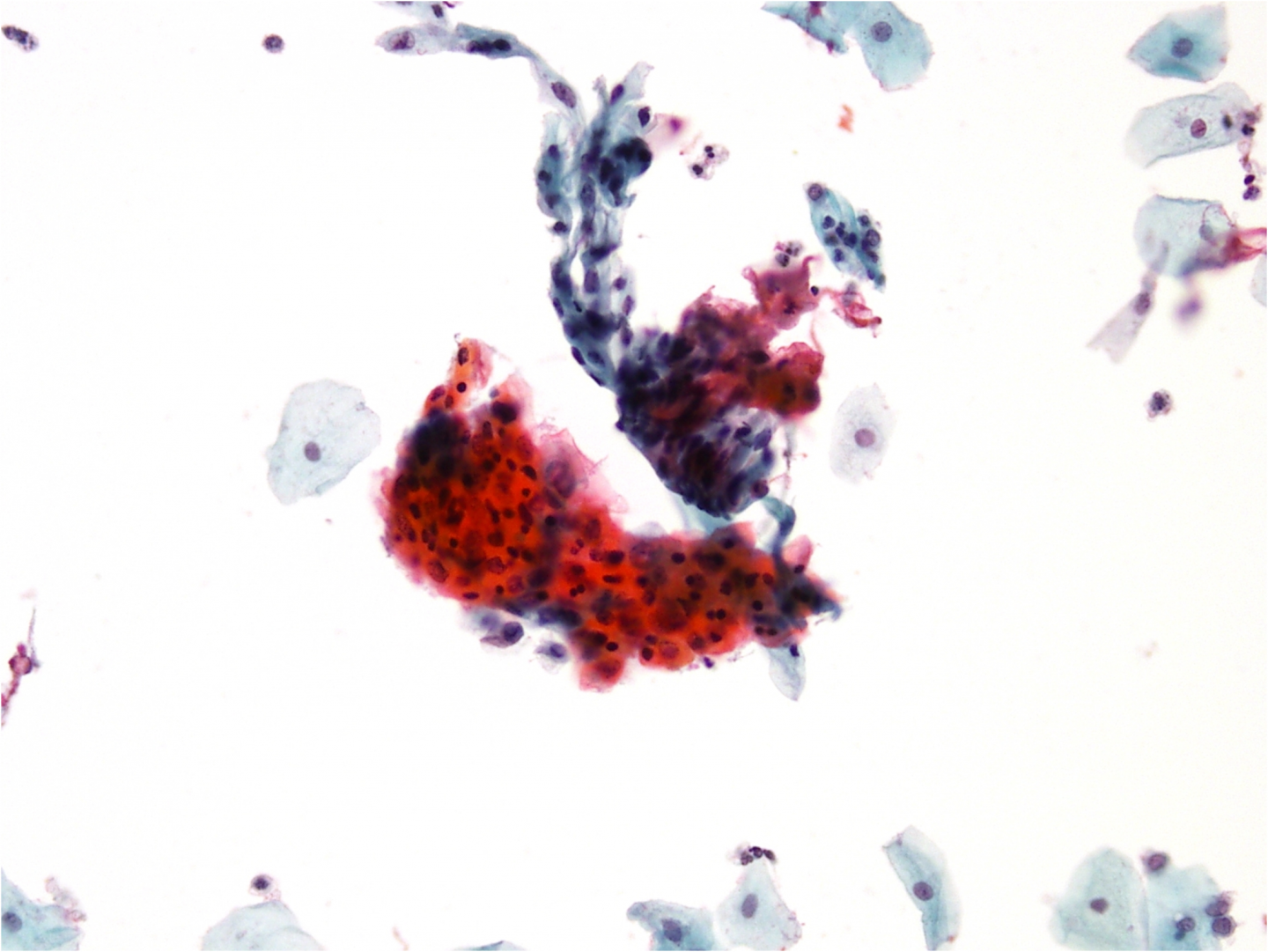
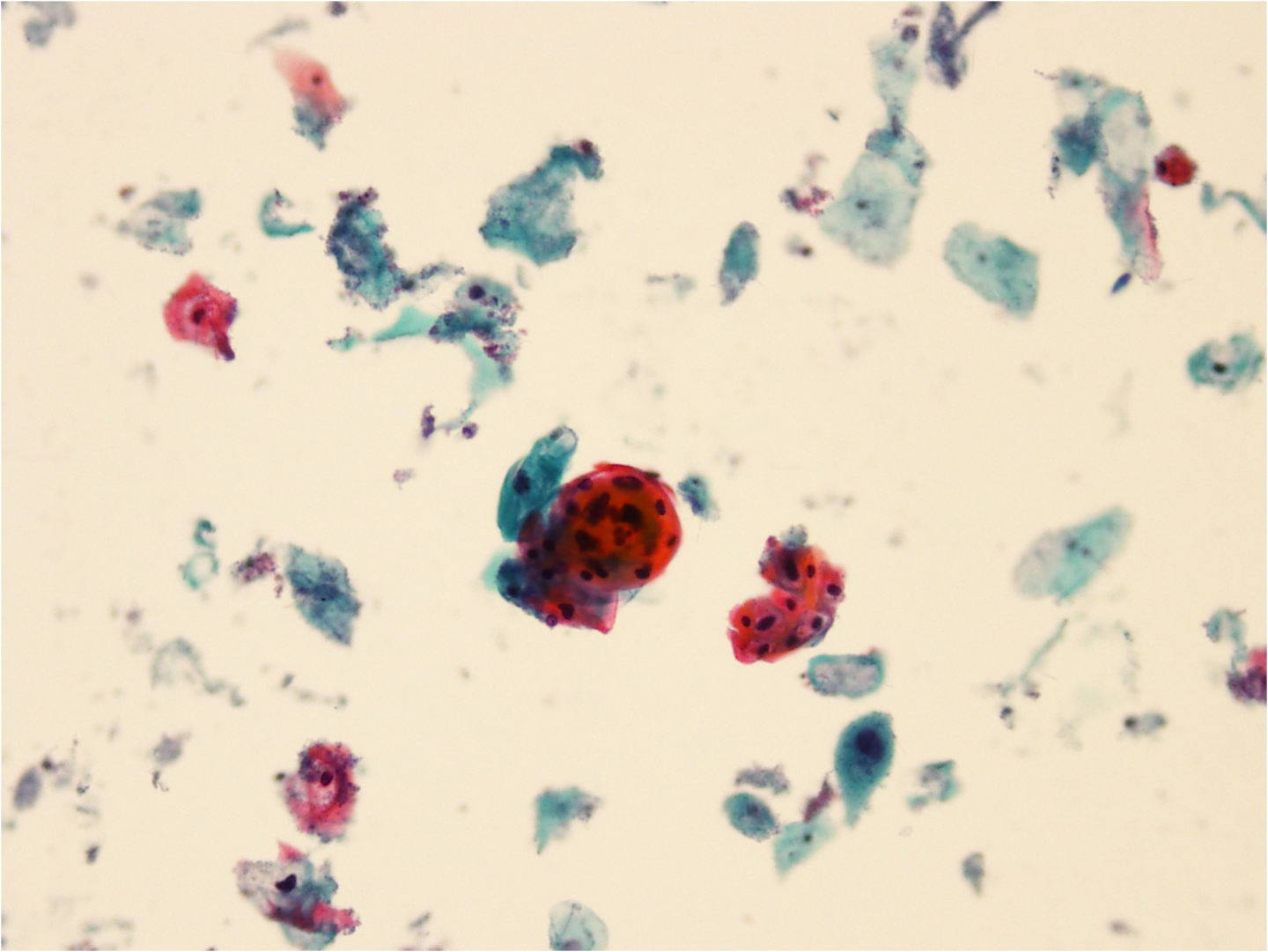
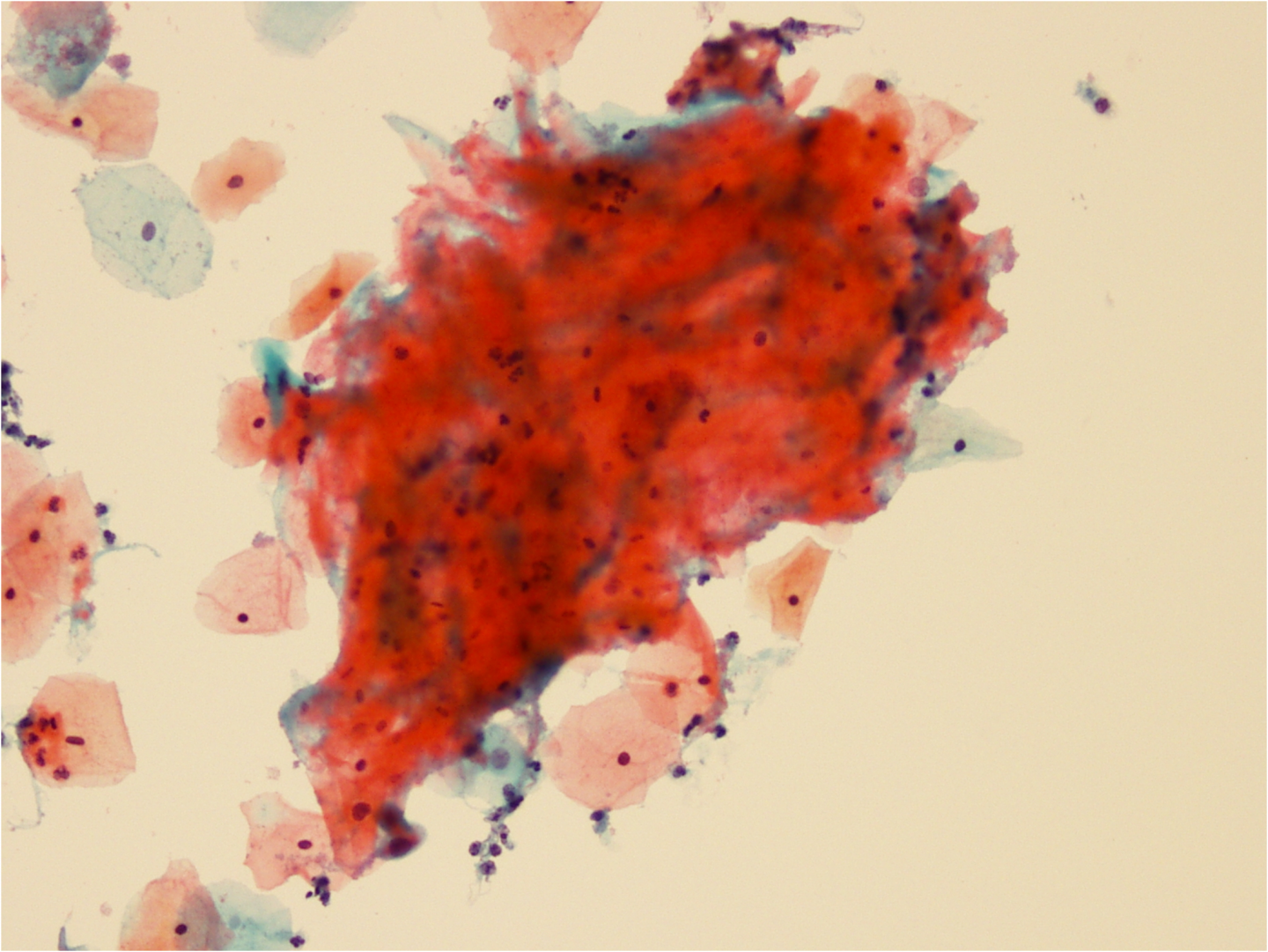
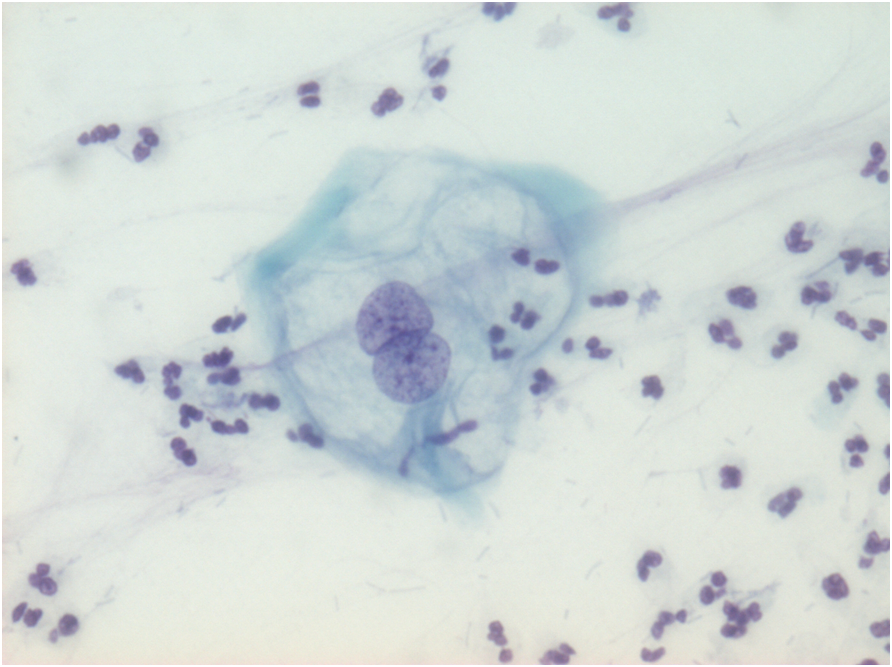
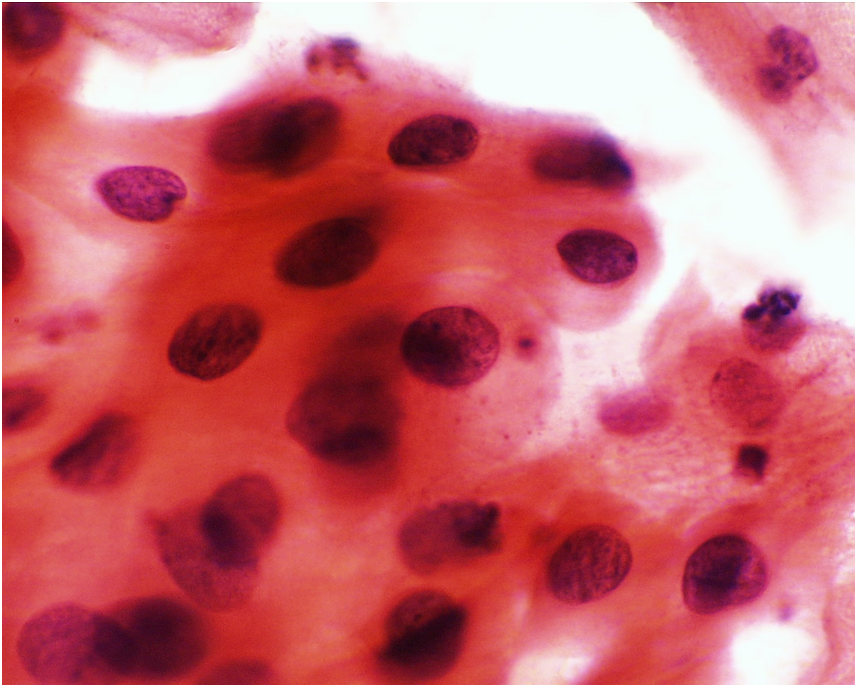
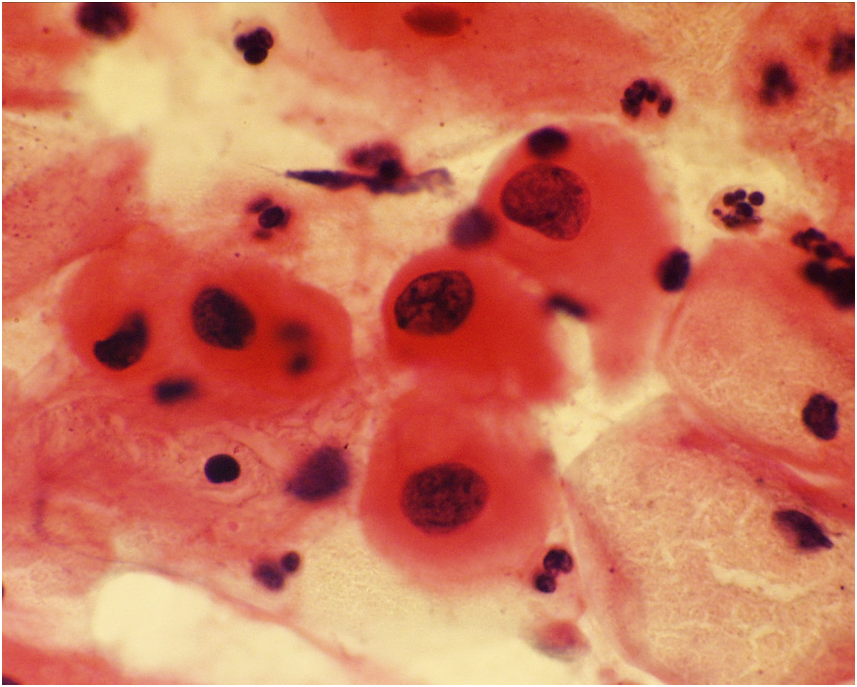
Double nuclei, multinucleation, parakeratosis, dyskeratosis and hyperkeratosis may all be seen in HPV infection but are non-specific when koilocytosis is absent (Figure 9c-4 a-d).
Koilocytes may occasionally be seen with nuclei that appear to be normal: these are sometimes classified as ASC-US or borderline if only one or two such cells are seen and other features of HPV absent (Figure 9c-4 f). HPV triage should be helpful in such cases, which may be caused by low-risk types of HPV (Steinman et al. 2008).
Dyskeratotic cells that have dense orangeophilic cytoplasm with very slight nuclear changes show that there is an irritant present on the cervix, which may or may not be HPV (Figure 9c-4 c-d). Cells like this should make you slow down and look for an explanation for their presence such as Candida albicans, which may produce similar changes, or more definitive features of HPV elsewhere.
Squamous pearls are parakeratotic cells that have curled up and formed a pearl-like structures. One or two such cell groups, without nuclear enlargement or anisocytosis, is unlikely to be important but seeing a large number (10+) could indicate an abnormality and a search for other abnormalities elsewhere on the slide.
Anucleate squamous cells are squamous with a ghost outline of a nucleus. They are a normal feature of keratinising squamous epithelium such as seen in the vulva. Their presence as isolated cells in a cervical smear is unlikely to be significant and is usually seen in otherwise normal samples. However, if present as several large clusters they indicate hyperkeratosis and may be associated with LSIL and occasionally HSIL, which should be looked for elsewhere on the slide (Williamson et al. 2003).
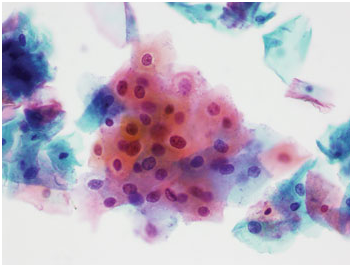
Figure 9b-4 (a-e). ASC-US with features often seen with HPV infection.
(a) Squamous cells showing parakeratosis, some variation in nuclear size and shape. Nuclei are small and hyperchromatic nuclei and some have double nuclei.
ASC-US in which distinction from non-specific inflammation or cannot be made with certainty
Samples from perimenopausal women may show nuclear enlargement without definitive features of LSIL. HPV infection is less common in older women and HPV triage can distinguish high-risk HPV-related SIL from normality (Steinman et al. 2008). With experience many such cases may be reported as normal.
Figure 9c-5
(a-b) Nuclear enlargement in a peri-menopausal sample reported as borderline: HPV status not known in this case but follow up was negative.