Clinical features
- Account for half of paediatric/adolescent sex cord stromal cell tumours
- Children and young adults
- 80% before age of 20 years
- Sexual precocity and irregular uterine bleeding (due to oestrogen production)
- Association with enchondromatosis (Ollier’s disease), Mafucci syndrome, infantile dimorphism and ambiguous genitalia
- 2% are bilateral
- Abdominal distension, pain or ascites
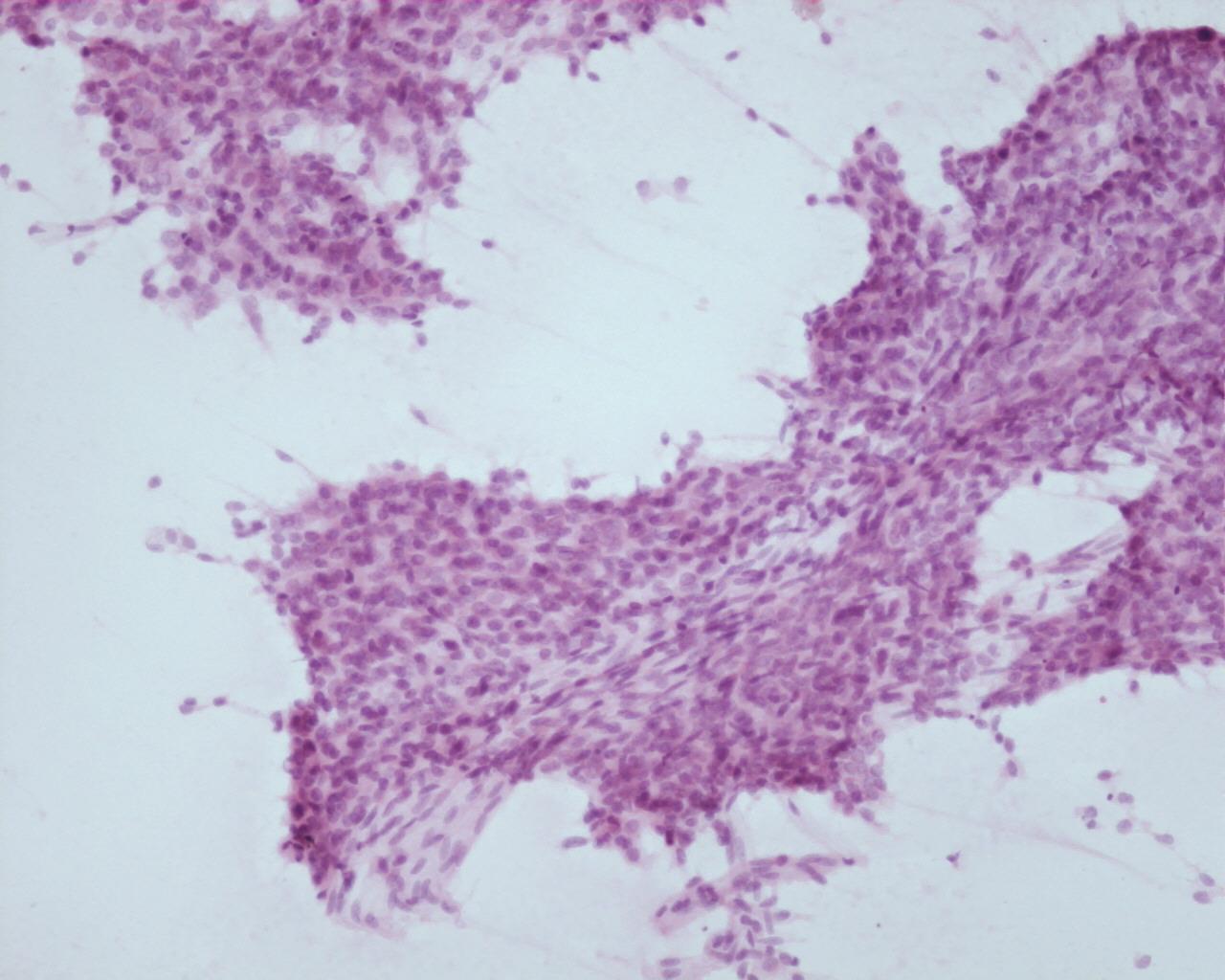
Fig 101 – Juvenile granulosa cell tumor- Loose clusters of homogeneous neoplastic cells (H&E)
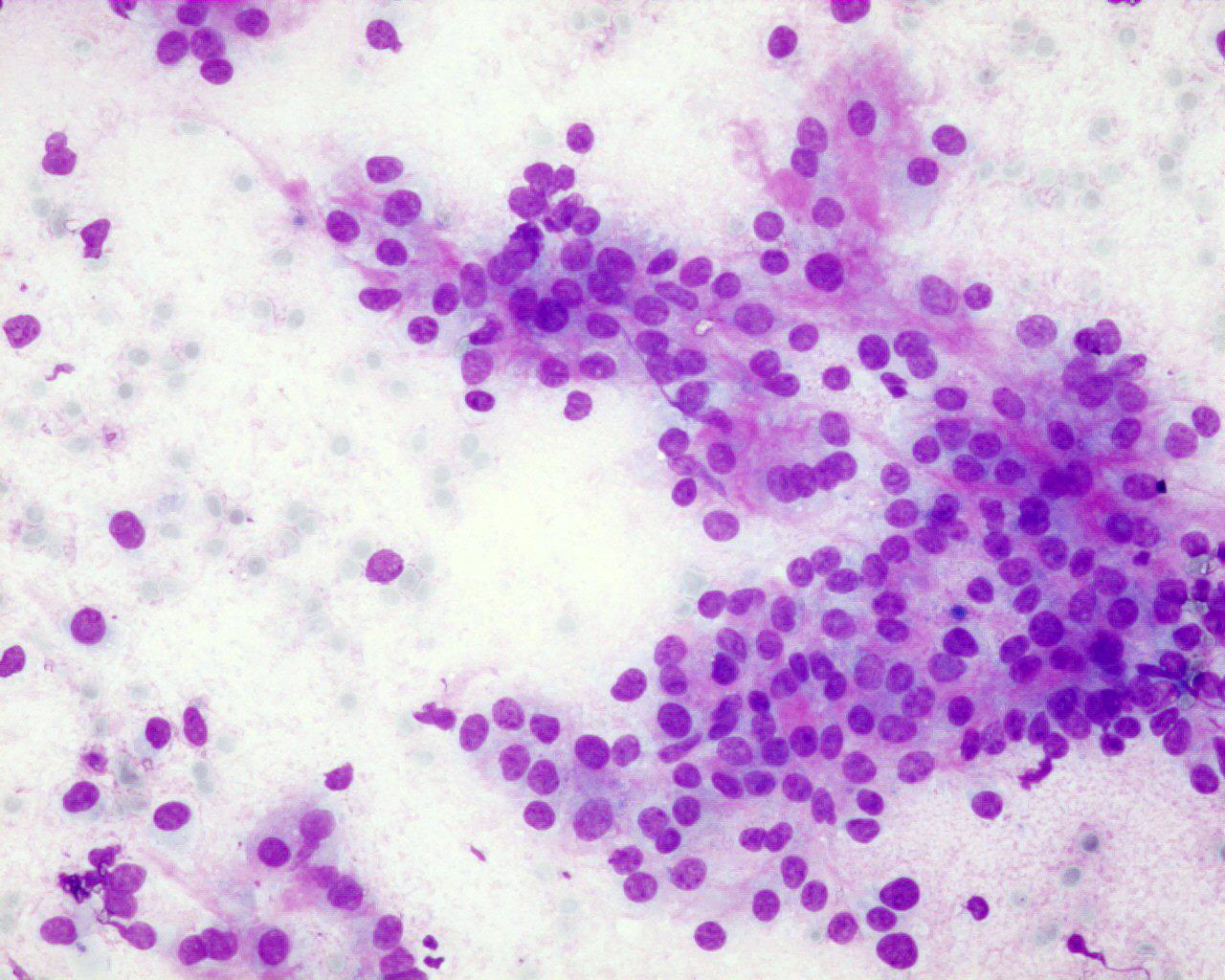
- Cellular smears
- Granulose cells
- In loose clusters or single
- Homogeneous round centrally placed nuclei
- Nuclei with fine chromatin
- Conspicuous nucleoli
- Paucity of nuclear grooves
- Atypia may be present
- Pale and vacuolated cytoplasm
- Indistinct cell borders
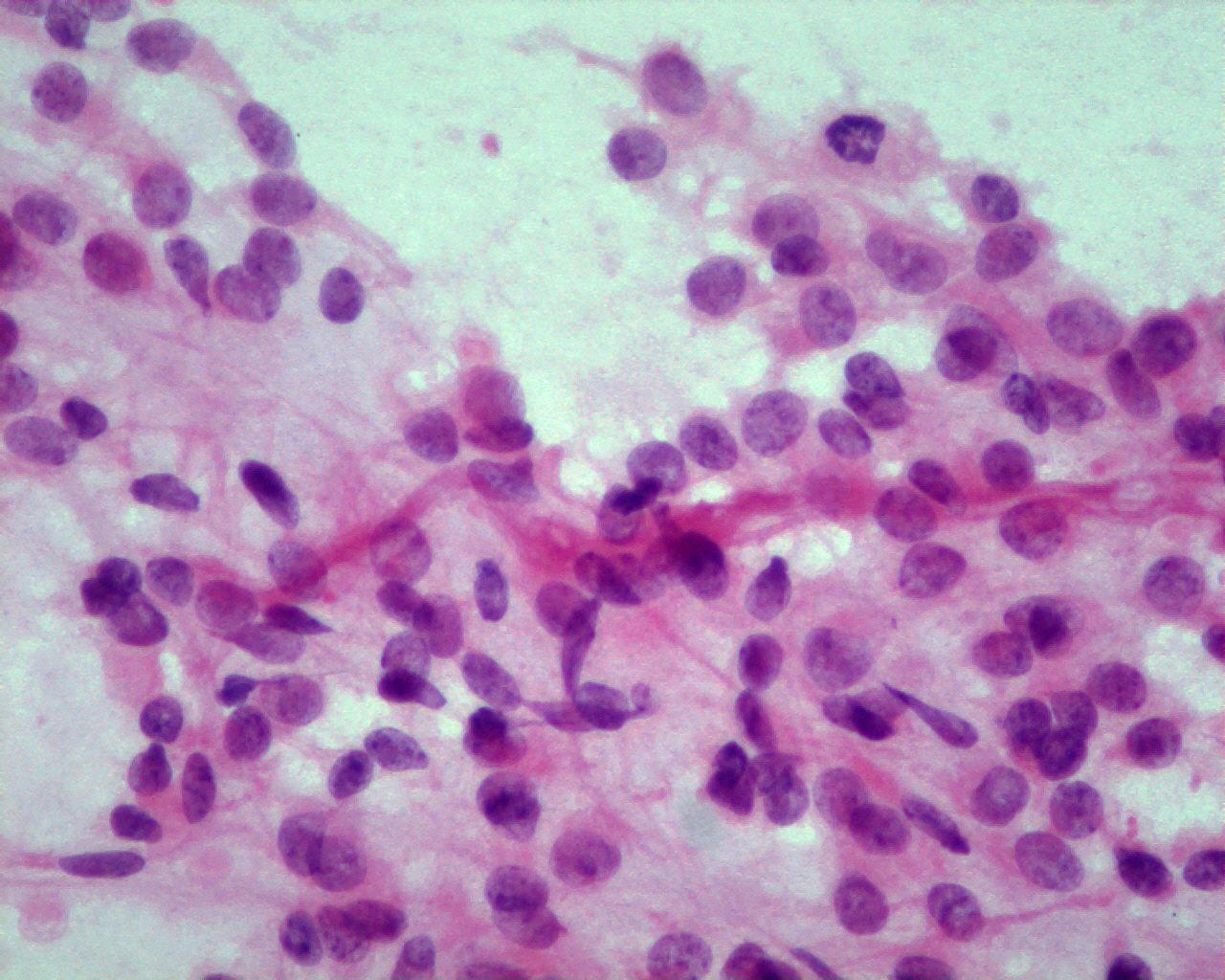
- Theca cells
- Elongated cells
- Hyperchromatic nuclei
- Macrophages
Immunocytochemistry
- Inhibin: positive (granulose cells)
- Calretinin: positive
- EMA: negative
- Vimentin: positive
- Smooth muscle actin : positive in theca cells
Electron microscopy
- Prominent smooth endoplasmic reticulum
- Numerous mitochondria
- Large lipid droplets in cytoplasm
Genetic studies
- Trisomy 12 (common to other stromal cell tumours)
Differential diagnosis
- Adult granulose tumour
- Nuclear grooves
- Less luteinized cytoplasm
- Yolk sac tumour/ embryonal carcinoma
- Granulose cell atypia is more pronounced than in yolk-sac or embryonal carcinoma
- Inhibin: negative
- Alpha-fetoprotein: positive
- Fibroma/ thecoma
- Rare in children
- Spindle cells intermingled with luteinized cells
Main points
- Most tumours are benign
- Propensity for late recurrence
- Prognostic factors: stage, size, rupture, nuclear atypia and mitotic activity