Clinical features
- The adrenal cortical cell is part of endocrine epithelia and has the capacity of hormone production: steroids, glucocorticoids and mineralocorticoids.
- Adenomas-rarely functional- incidental detection more frequent
- Carcinomas- 50% are hormone secreting – Cushing syndrome or virilisation of women patients (androgen secretion).
- 0.2% of all paediatric malignancies.
- Presentation and prognosis differ from those of adults
- More common at ages of 0-5 years, but presents bimodal occurrence: In infancy and in adolescence
- Abdominal mass with pain and fever
- Associations with Li-Fraumeni, Beckwith-Wiedemann, Ver-Morrison, cancer family syndrome, SBLA (S- sarcoma; B- breast and brain neoplasm; L- leukaemia, laryngeal and lung carcinoma; A- adrenal cortical carcinoma) and foetal alcohol syndrome
- Associations with genitourinary anomalies, neurofibromatosis, pigmented nevi, brain tumours and hemi hypertrophy
- Associations with endocrine abnormalities (virilisation and Cushing’s syndrome) is common in children, although feminization and Conn’s syndrome are rare
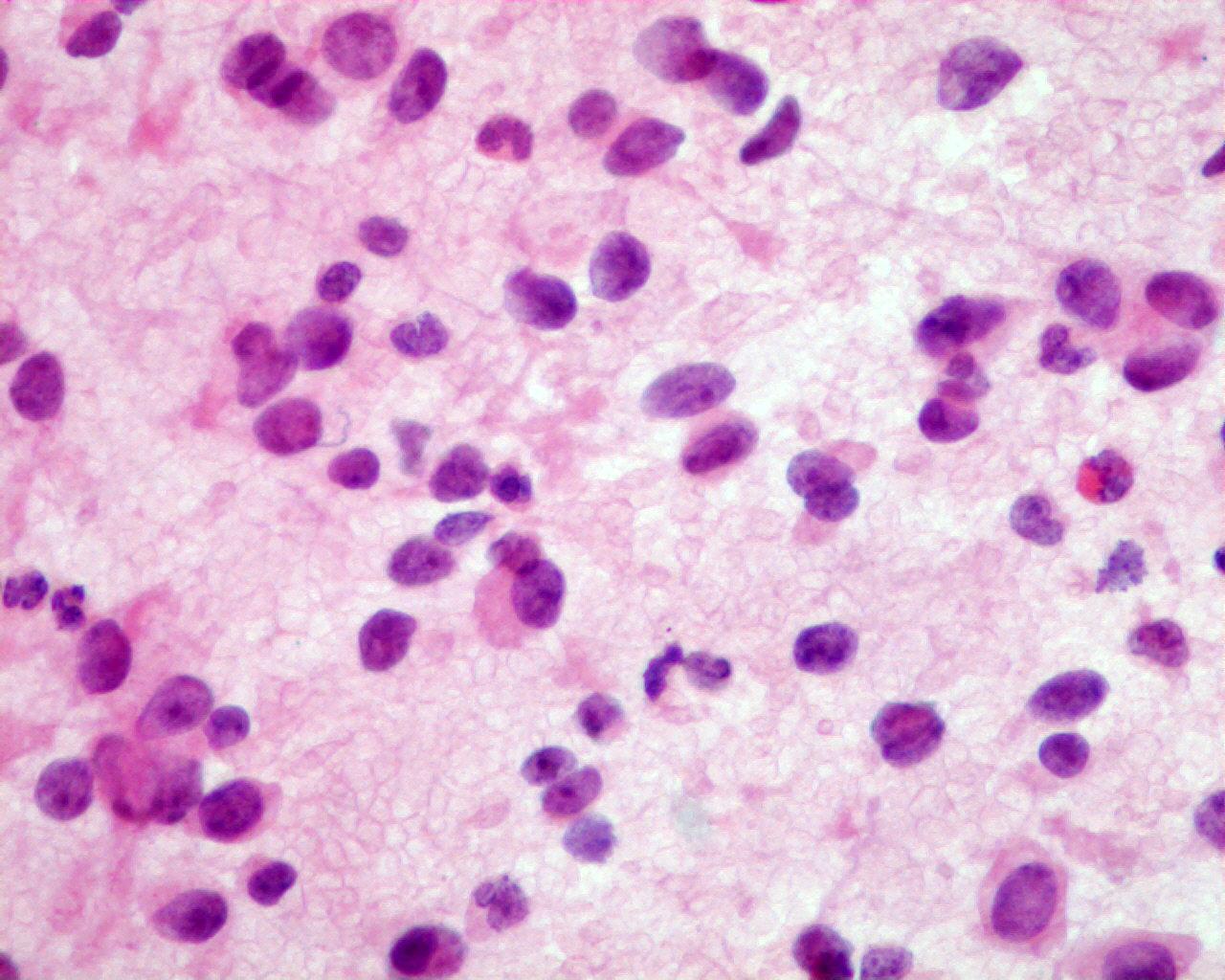
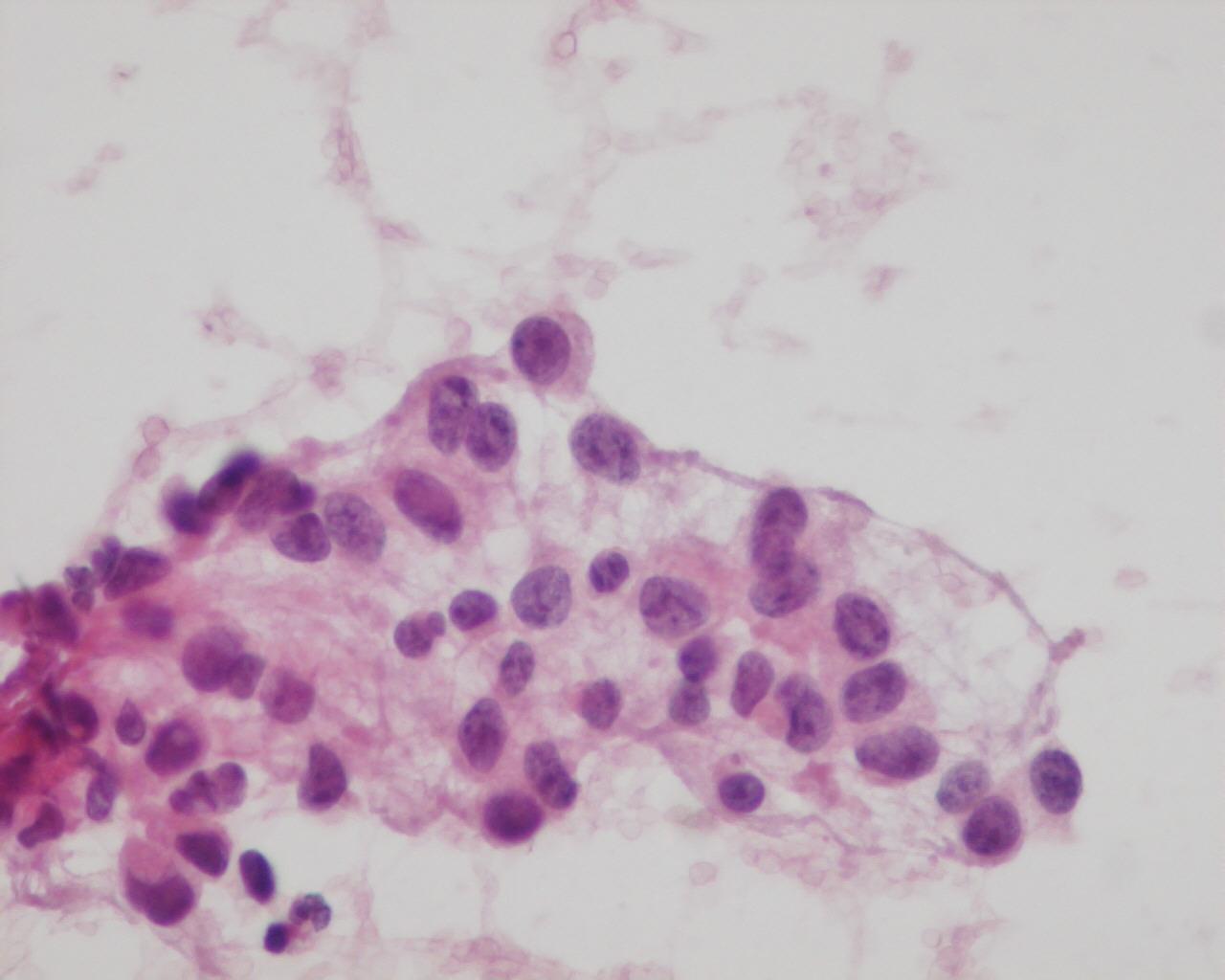
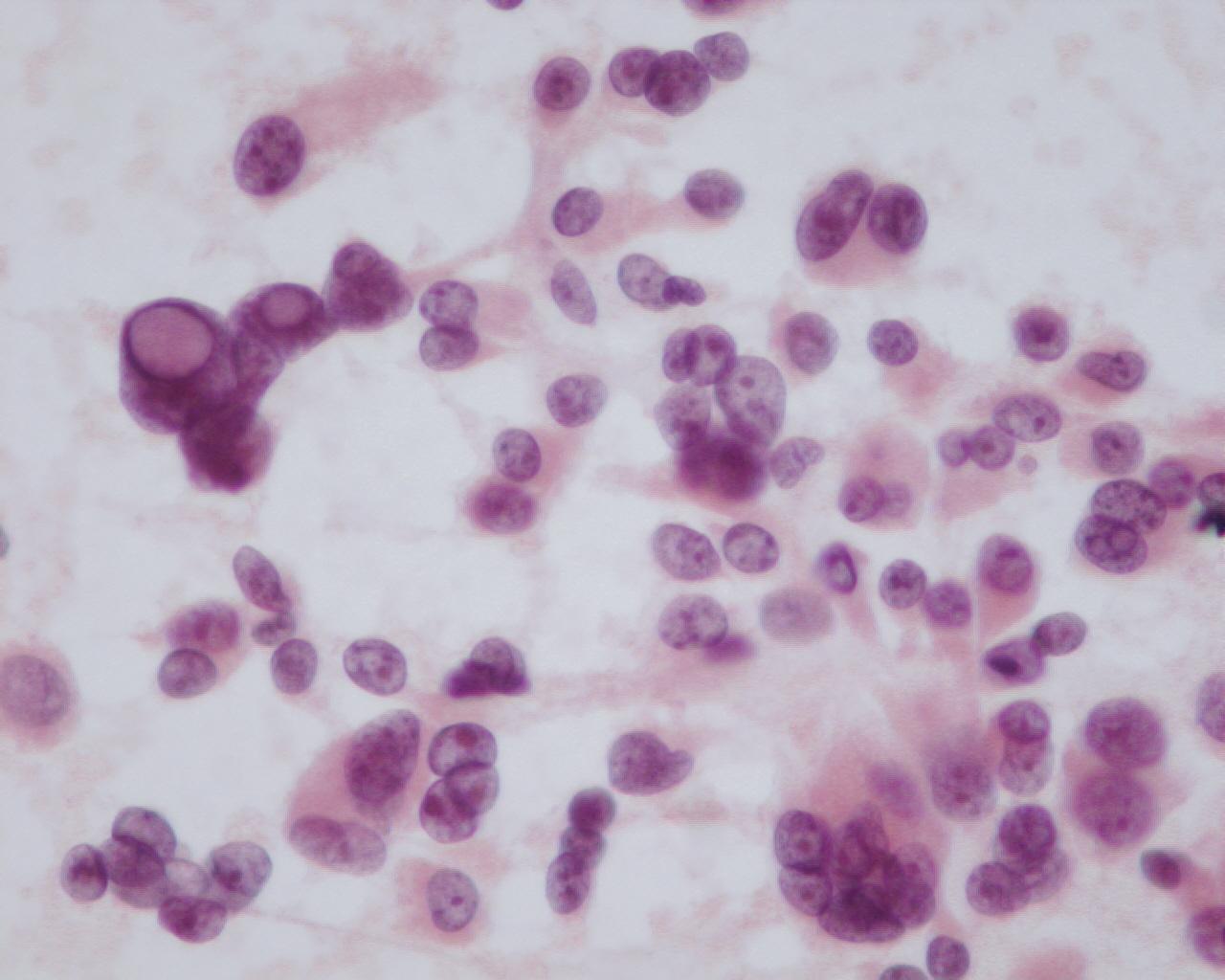
Fig 97 – Adrenal cortical adenoma/ carcinoma – Fine needle aspiration from an adrenal adenoma. Cellular smear with discohesive neoplastic cells with bland nuclei (H&E)
- Cellular smears
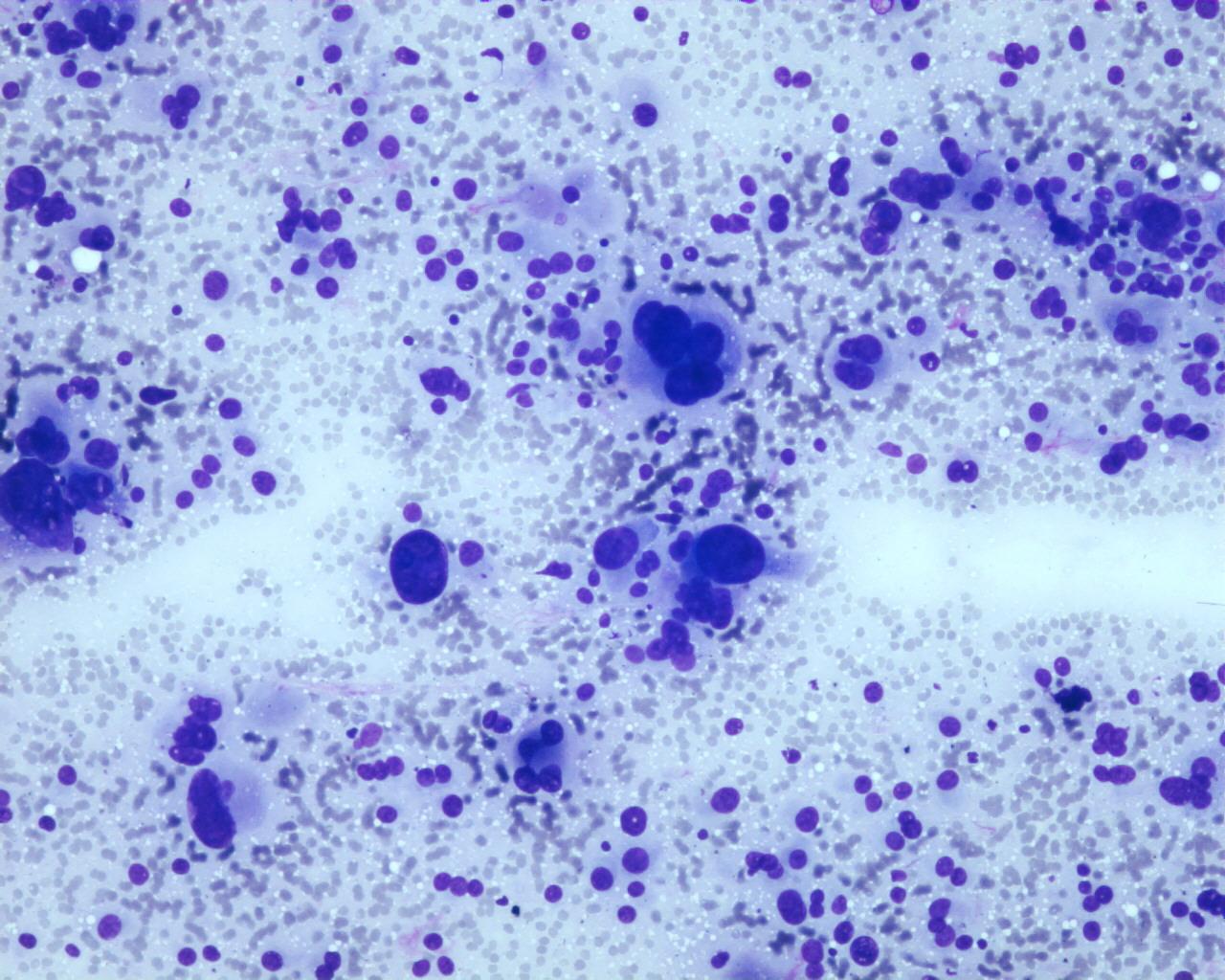
- Lipidic background-Giemsa stains
- Nude nuclei (single or in morular pattern)
- Sheets and discohesive neoplastic cells separated by delicate vessels
- Monomorphic cells with bland nuclei and pleomorphic cells, with irregular outline, coarse chromatin and evident nucleoli
- Neoplastic cells are polygonal or plasmacytoid
- Pleomorphism can be exuberant- not associated with malignancy
- Nucleoli can be prominent
- Eccentric nuclei
- Nuclear pseudo inclusions
- Cytoplasm ranging from eosinophilic (more frequent in carcinomas) to clear and vacuolated (more frequent in adenomas)
- Cytoplasmic hyaline globules
- Mitoses are variable
- Sarcomatoid appearance generally seen in poorly differentiated carcinomas
- There are no cytological criteria for distinguishing benign from malignant cases, although a bubbly lipid background has been reported by some authors to correlate with benign nature(7)
Immunocytochemistry
- D11: positive (nuclear) in 80%
- Ad4BP (nuclear adrenal 4 binding protein): positive (100% in adrenal cortical carcinomas)
- A103 (melan A): positive (100% in adrenal cortical carcinomas )
- Cytokeratin: decreased expression relative to the degree of malignancy
- Vimentin: increased expression relative to the degree of malignancy
- Inhibin A: positive
- NSE: positive
- Synaptophysin: positive
- Chromogranin: negative
- CAM 5.2:positive
- S100 protein: positive
- Hep Par1: positive
- CEA: negative
- EMA: negative
- CD10: negative
- CK7: negative
- CK20: negative
- HMB45:negative
- Bcl-2: positive
Differential diagnosis
- Renal cell carcinoma
- More discohesive cellular smears
- Well-defined polygonal cells with centrally placed nuclei
- Prominent nucleoli
- Pleomorphism, when seen, is more uniform in the cell population
- Low molecular weight cytokeratin: positive
- EMA: positive
- CD10:positive
- D11: positive (occasionally)
- Ad4BP: negative
- A103 (melan A): negative
- Inhibin A: negative
- Neuroendocrine markers: negative
- CEA: negative
- Hepatocellular carcinoma
- Low molecular weight cytokeratin: positive
- D11: positive in 100%
- Ad4BP: negative
- A103 (melan A): negative
- Inhibin A: negative
- Neuroendocrine markers: negative
- Pheochromocytoma
- Chromogranin: positive
- Bcl-2: negative
- Inhibin A: negative
- EMA: negative
Main points
- Functional tumours do not carry worse prognosis, unlike in adults
- A poor outcome is more common in the adolescent age group
- Survival, in malignant cases, depends on the stage and the completeness of surgical resection
- Children with Beckwith-Wiedemann Syndrome have better prognosis (6) There are no cytological criteria for distinguishing benign from malignant cases, although a bubbly lipid background has been correlated by some authors with benign nature