Clinical features
- Infants and children. Approximately 20% are congenital, and more than 50% are diagnosed under 12 months
- Benign solitary cutaneous lesion composed of histiocytes
- Location-subcutaneous or deep seated ( 5% of the cases)
- In 4% of the cases systemic distribution is referred
- Multiple lesions in 12% of the cases
- Upper part of the body (head, neck, upper trunk and extremities) is most commonly involved
- Cases reported in eye, heart, bone and lungs are also reported, even though exceptional
- Association with neurofibromatosis Type I or juvenile myelomonocytic leukaemia in rare cases , epilepsy, Nieman-Pick disease, urticaria pigmentar and CMV infection
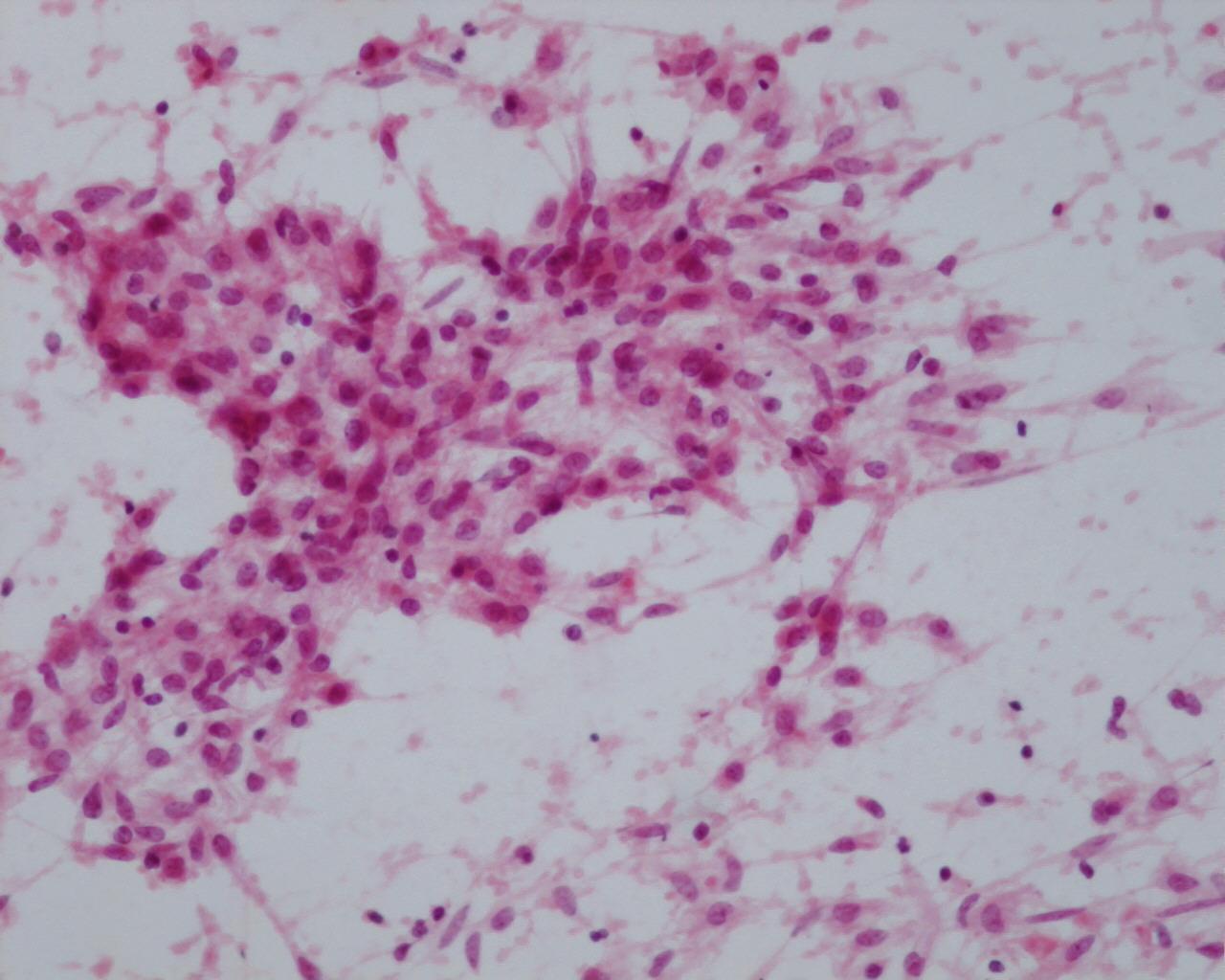
Fig 58 – Juvenile Xanthogranuloma –Numerous histiocytes in a loosely cohesive group, is simulating a granulomatous arrangement. Inflammatory cells dispersed in the background (H&E)
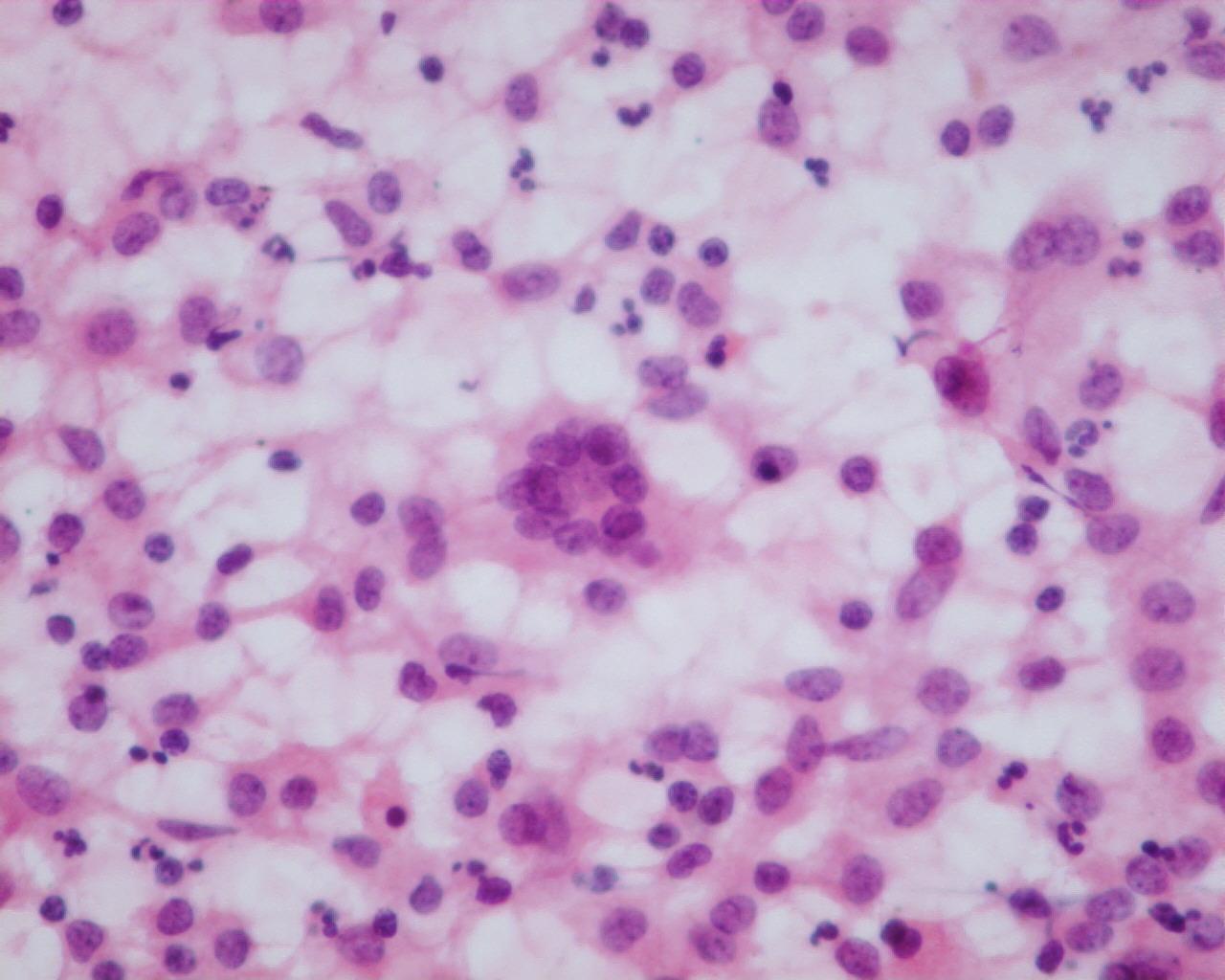
- Cellular smears, with vacuolated material in the background ( Diff-Quick)
- Loosely cohesive monotonous histiocytic cells
- Oval nuclei, that can occasional bare a notch
- Hypodense cytoplasm with occasional lipidic-like vacuoles
- Lymphocytes, macrophages and polimorphonuclear cells (neutrophils and/or eosinophils in variable quantities)
- Multinucleated cells, sometimes with Touton –like appearance
- Necrosis can be present
- Variable number of mitosis
Immunocytochemistry
- CD68: Positive
- Factor XIII: Positive
- Fascein: Positive
- CD14: Positive
- CD163: Positive
- CD4: Positive (occasional)
- Vimentin: Positive ( focal )
- S100-protein: Negative
- CD1a: Negative
Modern Techniques of Diagnosis
- Non-contributory
Differential Diagnosis
- Granulomatous inflammatory lesions
- The presence of mycobacterium or fungi must be excluded.
- Langerhans ‘cell histiocytosis
- Typical indented nuclei with a notch
- CD1a and S100-protein are positive
- Electron microscopy : Birbeck granules
- Xanthoma
- Typically associated with hiperlipidemia
- Frequent cytoplasmic lipidic vacuoles
Main points
- Pathogenesis remains uncertain- more probably a pseudoneoplastic condition
- Histogenesis is still controversial- dermal dendritical cells?; plasmacytoid monocytes
- Spontaneous regression over time, (1/3 before 6 months, 1/3 between 6 and 12 months and 1/3, between 12 months and three years