Clinical features
- Mainly affect adolescents and young adults
- No sex predilection
- One-third of cases has a major nerve involvement with neurological symptoms
- Common sites: paravertebral region, lower extremities and retroperitoneum
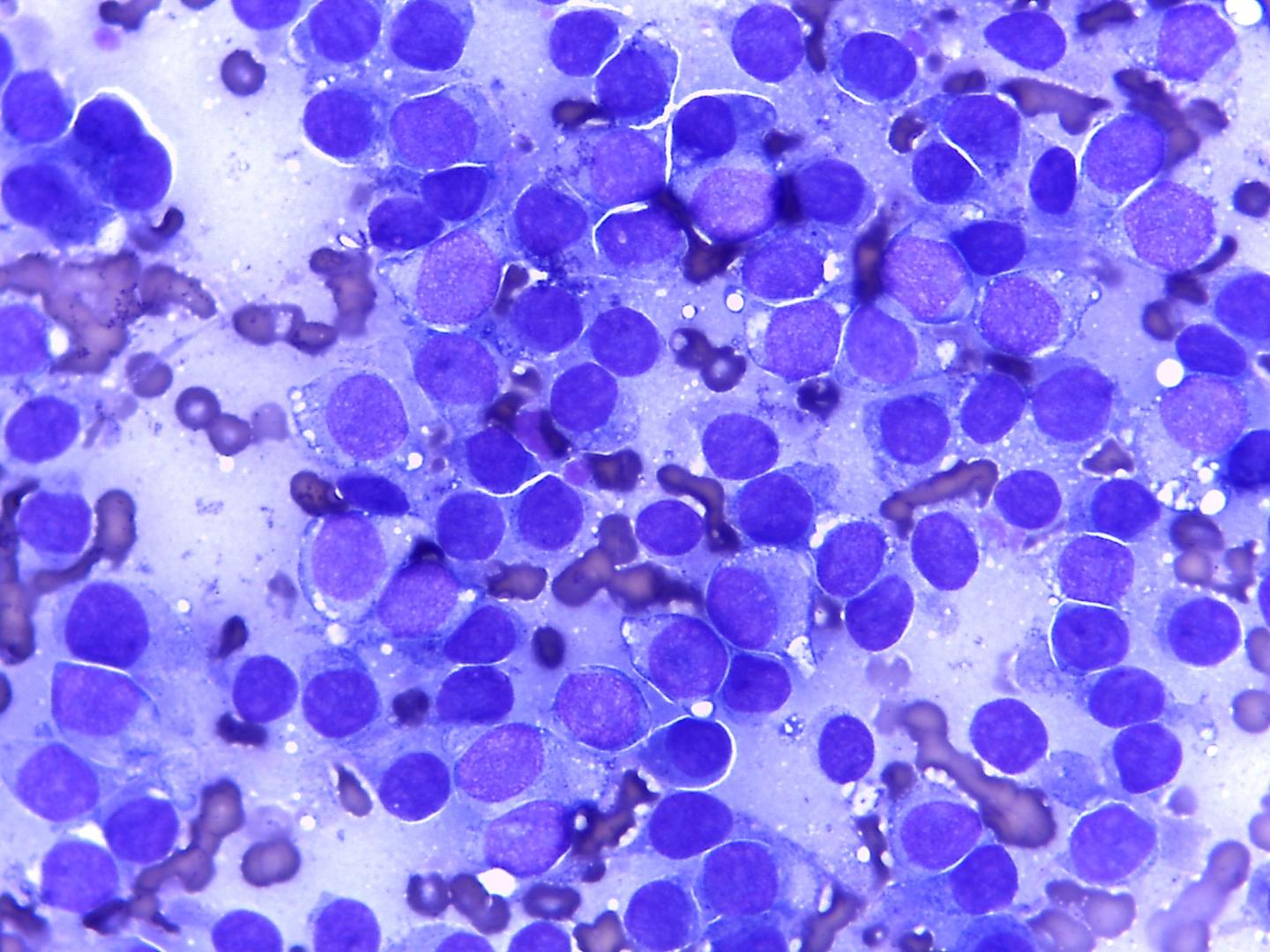
Fig 50 – PNET – Discohesive monomorphic small round cells. Tigroid background (Giemsa)
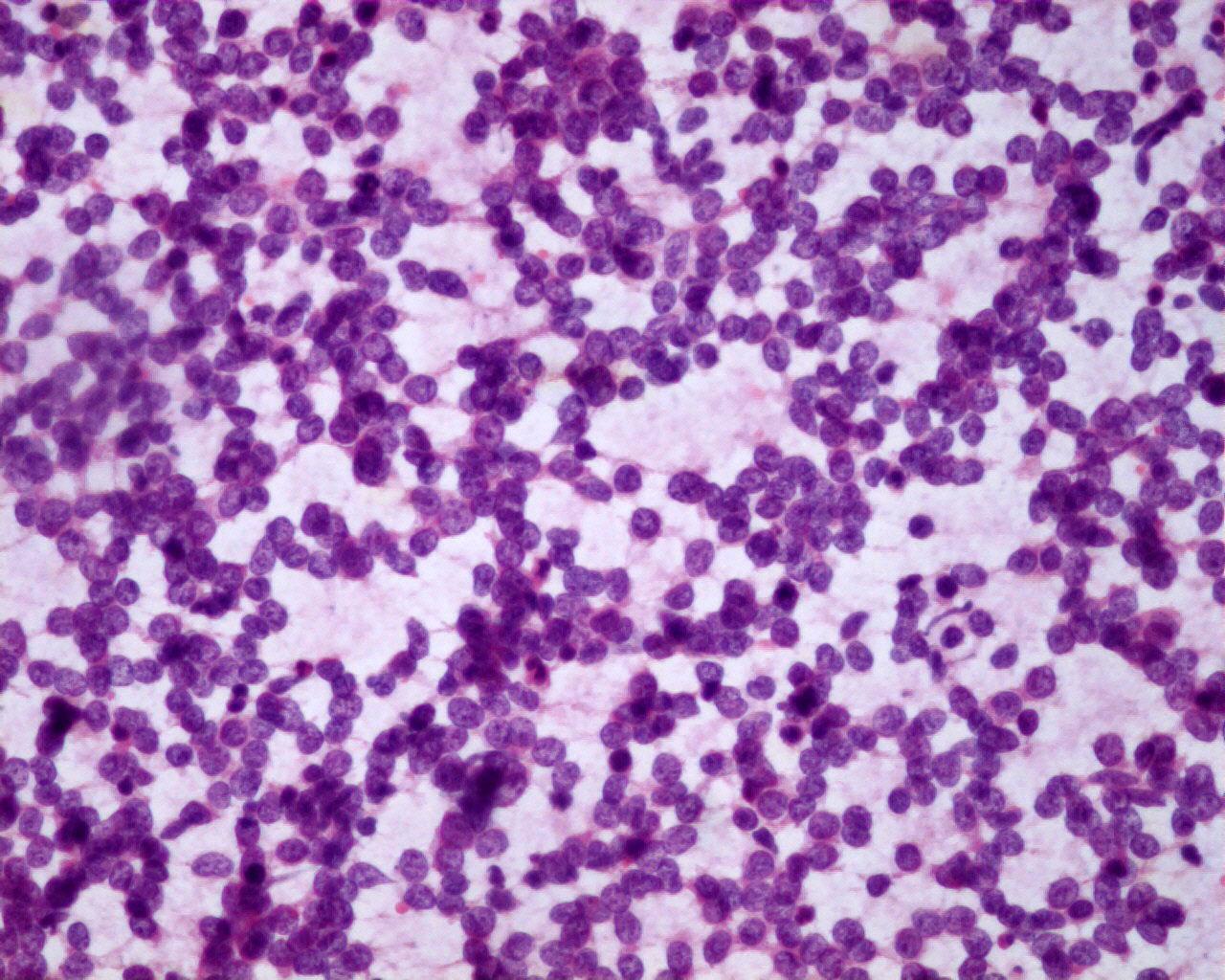
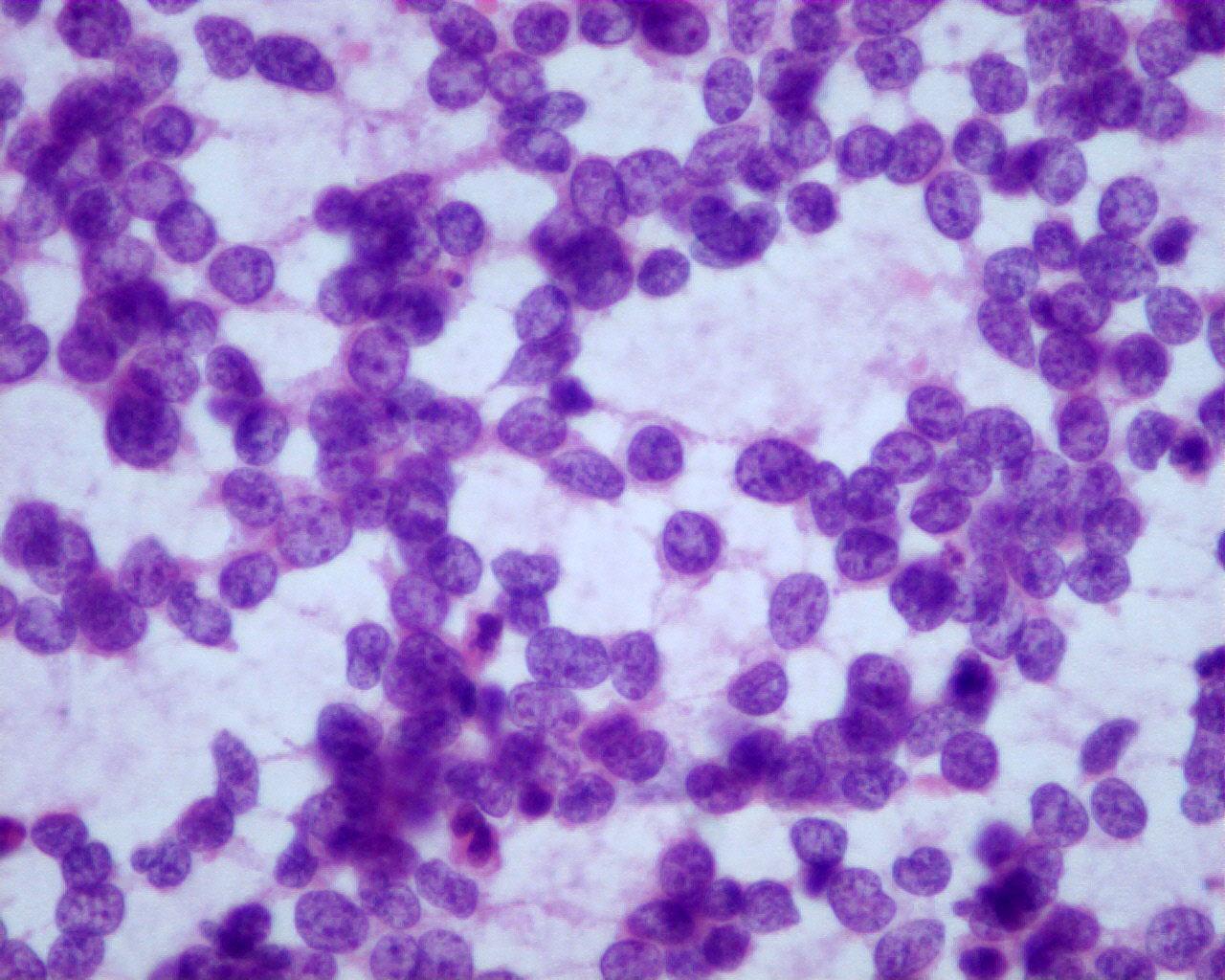
- Discohesive or in groups of monomorphic small round cells
- Dimorphic population of smaller and darker cells and lighter staining cells
- Lighter cells have
- Pale chromatin and small nucleoli
- Membranous cytoplasmic blebs (Diff-Quick staining)
- Darker cells have condensed chromatin and scarce cytoplasm (they are probably cells in degeneration)
- Absence of neuropil and ganglion cells
- Rosettes are seen, even though rarer than in neuroblastoma
- Tigroid background can be seen
- Necrosis
Immunocytochemistry
- CD56 (NCAM): negative
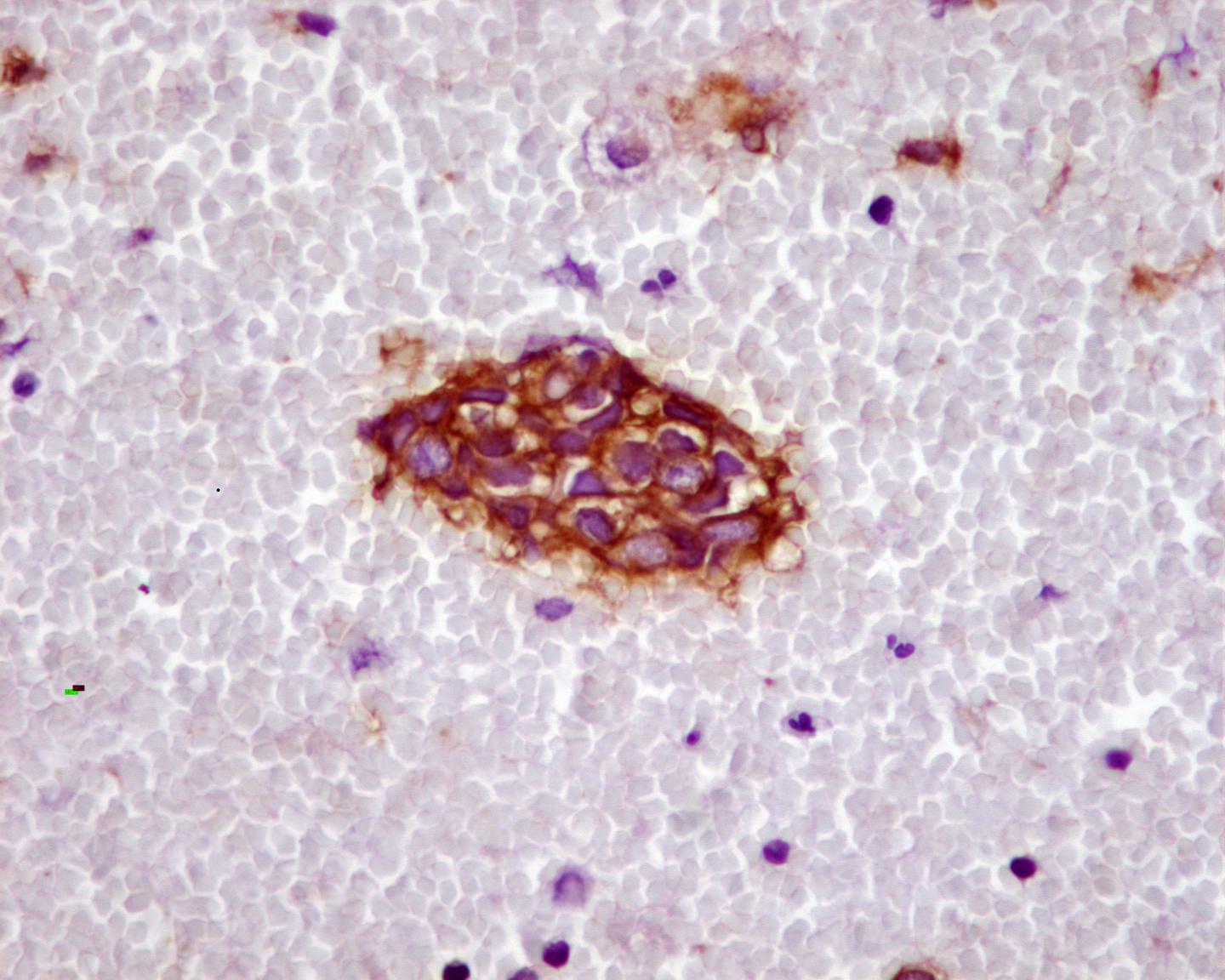
- CD99: positive (membranous pattern)-not specific but the most useful marker
- Caveolin-1 :positive, even in CD99 negative cases
- FLI-1 : positive (nuclear-only 70% of the cases)
- Cytokeratin’s: focal positivity in 20%
- CK20: negative – useful differentiating with Merkle tumour
- Vimentin: positive
- AE1AE3:positive
- P63: positive in some cases
| Synaptophysin: positive (focal)Chromogranin: in most cases negativeNSE: positive | Low diagnostic utility |
| List of CD99 positive tumours |
| Ewing/PNET |
| Alveolar rhabdomyosarcoma |
| Desmoplastic small round-cell tumour |
| Atypical teratoid rhabdoid tumour |
| Synovial sarcoma |
| Mesenchymal chondrosarcoma |
| Merkel cell carcinoma |
| Non-Hodgkin lymphoma |
Genetic studies
- t(11;22)(q24;q12) in 90% of the cases
- t(21;22) or t(7;22) – 15% of the cases
- C-myc over expression
- N-myc: no expression
Differential diagnosis
- Neuroblastoma
- Younger patients
- Usually secretes catecholamine’s
- Neuroblasts are generally present at different stages of differentiation
- Neuropil frequently present
- Rosettes frequently present
- Vimentin: negative
- Fli1: negative
- CD56 N-CAM: positive
- N-myc: may be over expressed
- No t(11;22)
- Atypical teratoid rhabdoid tumour
- Malignant central nervous system neoplasm
- In 2% of the cases located in the spine
- Huge nucleoli
- Rhabdoid cytoplasm
- Areas with eosinophilic cytoplasm globoid “inclusions”
- Para nuclear whorls of intermediate filaments(EM)
- EMA: positive
- Vimentin : positive
- Synaptophysin: positive
- MIC 2: positive- it may stain cellular membrane
- INI1: negative (rare cases of positivity in the CNS are described)
- 22q11 deletions
- Wilms´ Tumour
- In visceral (kidney) presentation of Ewing Family Tumours
- CD99: negative
- Alveolar rhabdomyosarcoma
- Actin: positive
- Rare cases of PNET may have myogenic differentiation (ectomesenchymoma)
- Desmin: positive
- Myogenin :positive
- CD99 may be positive (20-25%)
- Lymphoma
- Lymphoglandular bodies
- CD45: positive
- CD99: positive in lymphoblastic lymphomas (90%)
- CD3, Tdt and CD43: positive
- Neuroendocrine markers: negative
- Small cell osteosarcoma
- Presence of osteoid
- Neuroendocrine markers: negative
- Desmoplastic small cell tumour
- More frequent in an intra-abdominal location
- Divergent differentiation
- Wt1: positive
- Undifferentiated Synovial sarcoma
- EMA: positive (even in cases negative to other keratins)
- Keratins: positive, mainly high molecular weight cytokeratin’s (60-70%)
- CD99: positive in 50-100% in spindle and poorly differentiated pattern (absence of membranous pattern)
- Bcl-2: positive (79%)
Main points
- PNET/ Ewing´s Sarcoma-Well and poorly differentiated ends of a spectrum of round-cell sarcomas with a partial neuroectodermal phenotype-Ewing Family Tumours (EFTs)
- Neural crest origin
- 1% of all soft tissue sarcomas
- PNET and Ewing’s sarcoma are related entities and nowadays form a single group of bone and soft-tissue tumours (electron microscopic, immunohistochemical and cytogenetic features are remarkably similar)
- Surgical resection and/or radiotherapy and chemotherapy have increased survival from less than 10% to 40%
- Lack of responsiveness to preoperative chemotherapy
- Prognosis:
- Stage; site; size; age; response to therapy
- EWS exon7 fusion with FLI1 exon 6)- better prognosis
- Deletion 1p-poor prognosis
- P53 mutation – poor prognosis