Clinical features
- Frequent in the first two decades of life
- History of rapid growing (weeks)
- Most common locations: upper extremities, head, neck, chest or back
- Small size lesions-2-3 cm
- Subcutaneous, in children and young adults
- Rarely in neonates
- Previous trauma in 10% to 15%
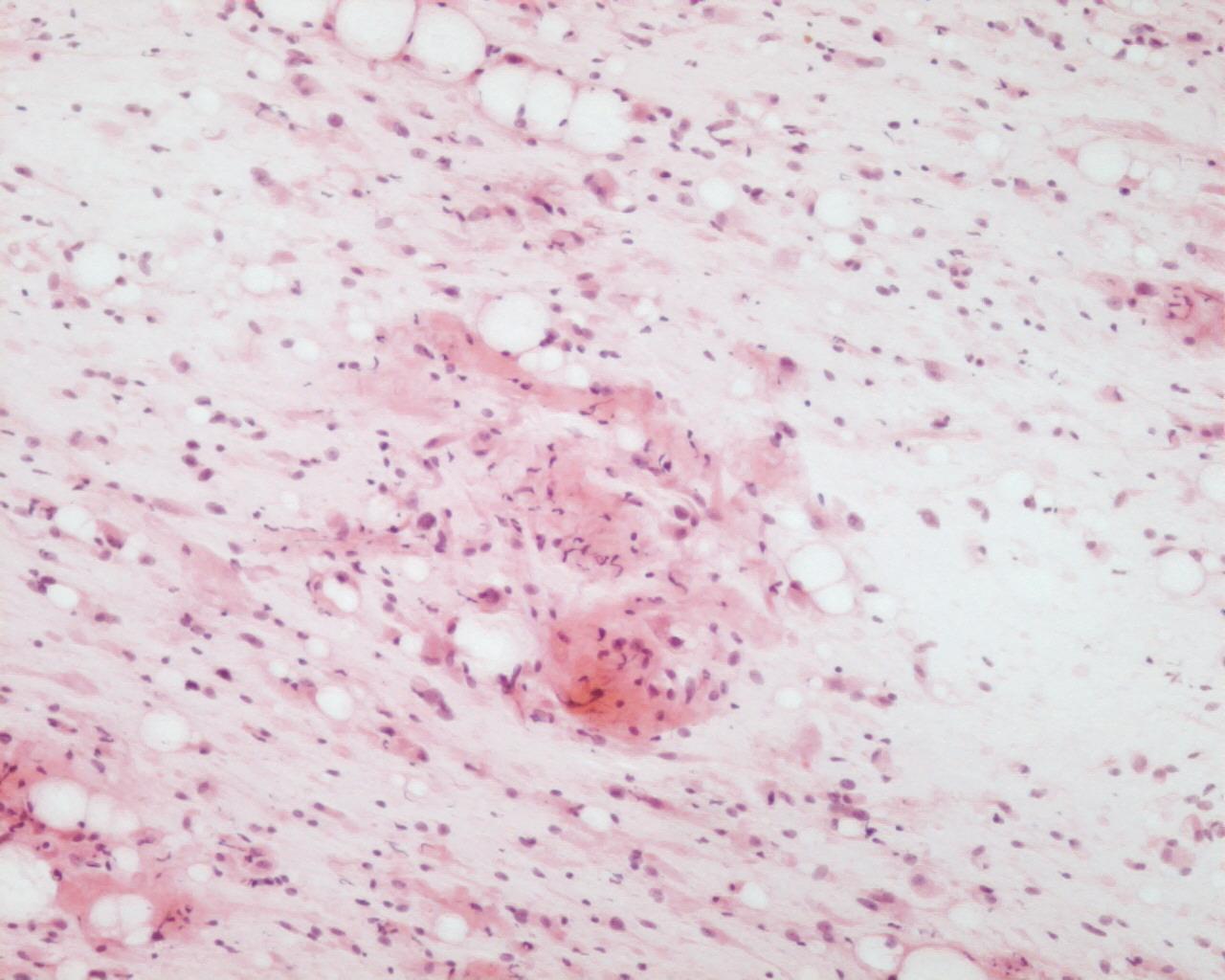
Fig 29 – Nodular fasciitis- Myxoid spindle cell lesion
- Hypercellular smear
- Recognition of a myxoid spindle cell lesion in 5% of the cases
- Dispersed to cohesive cells
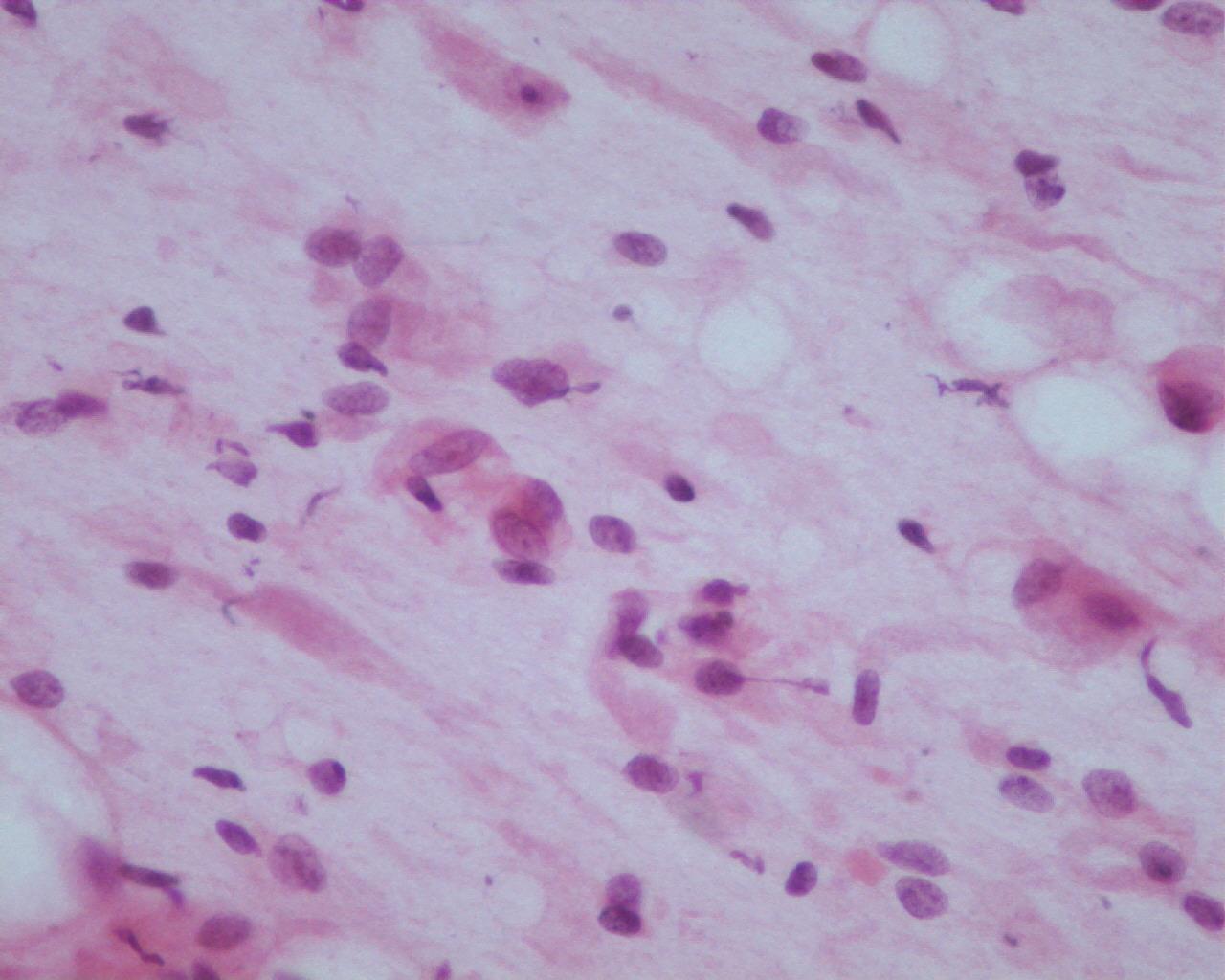
- Bland looking, but pleomorphic myofibroblasts (plump, spindle, ovoid, kidney-shaped nuclei)
- Binucleated forms
- Triangular cells
- Eccentrically placed nuclei with bland chromatin
- Ganglion cell-like
- Frequent mitosis
- Inflammatory cells (neutrophils, lymphocytes, eosinophils) histiocytes and/or multinucleated giant cells)
Immunocytochemistry
- Vimentin: Positive
- CD68: Positive
- Smooth muscle actin: Positive
- Calponin: Positive
- Desmin: Negative
- S100 protein: Negative
- CD34: Negative
Genetic studies
- MYH9-USP6 fusion gene
Differential Diagnosis
- Myxoid liposarcoma
- Lipoblasts
- Absence of inflammatory background
- Malignant fibrous histiocytoma
- More atypia
- Schwannoma
- Marked cellularity
- Less single cells
- Rare/no mitosis
- No inflammatory background
- Prominent stromal fragments with hypercellular and hypocellular areas
- Verocay bodies
- Palisade
- S100 protein: Positive
Main points
- Self-healing in 3-4 weeks
- Local excision can be an adequate treatment
- In conjunction with clinical presentation, cytology can be diagnostic