Clinical features
- Most frequent primary liver tumour in children (40% of all paediatric hepatic tumours and 55% of all malignant tumours)
- 88% occur at under 5 years of age; 68% during the first two years of life
- Male predominance
- More frequent in white patients
- 60-70% in right lobe
- Associations with: prematurity, low birth weight (< 1500 g), Beckwith- Wiedemann syndrome, trisomy 18 syndrome, familial polypoid adenomatosis and hemi hypertrophy
- 80-90% have significant elevation of serum alpha-fetoprotein
- lower levels of alpha-fetoprotein may indicate a poorer prognosis
- Paraneoplastic syndromes: thrombocytosis, human chorionic gonadotropin production (virilisation) and osteoporosis
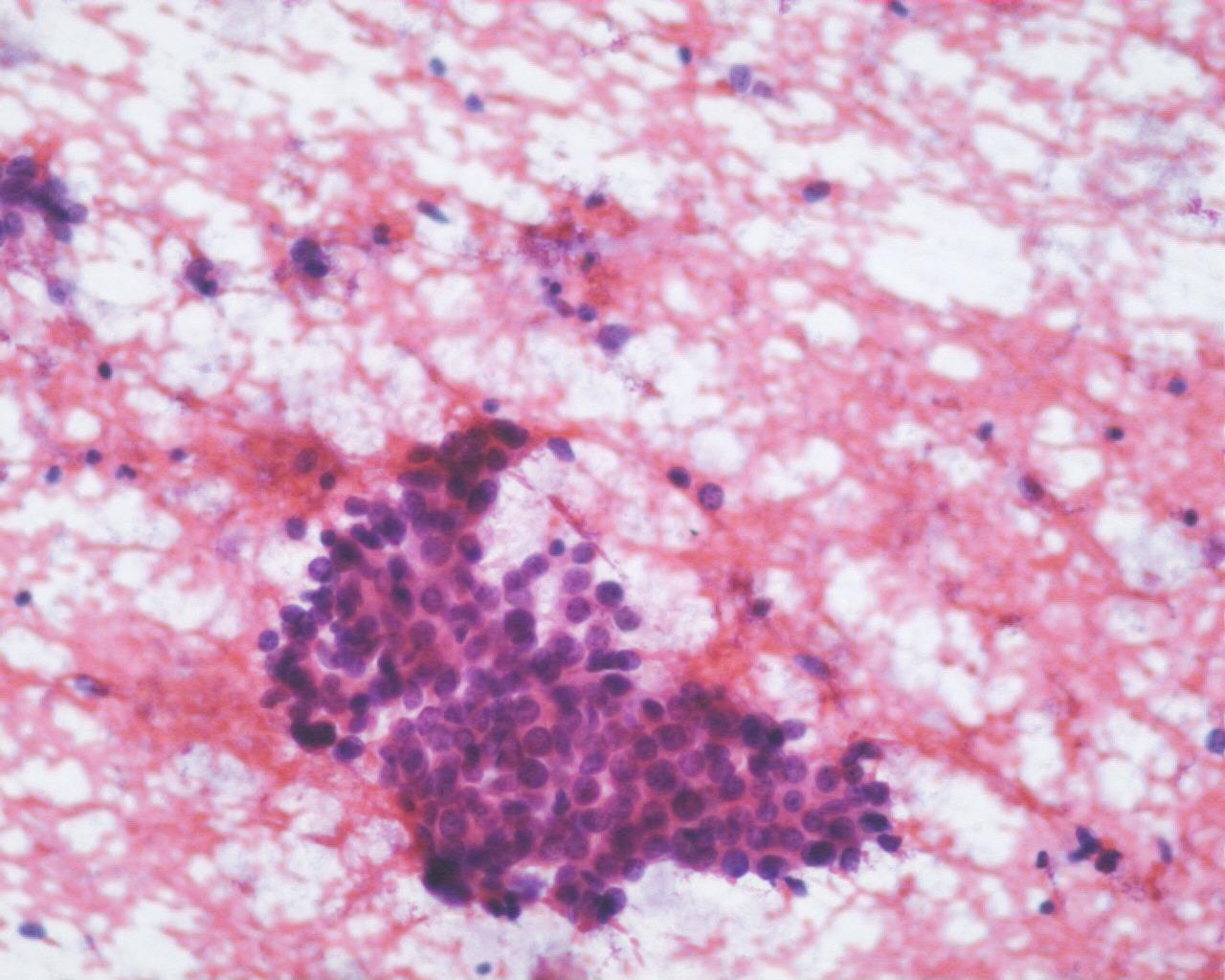
Fig 76 – Hepatoblastoma – Clusters of uniform small appearing cells with high N: C ratio (H&E)
- High cellularity
- Small hepatocytes with high N/C ratio
- Centrally placed nuclei
- Nucleoli may be prominent
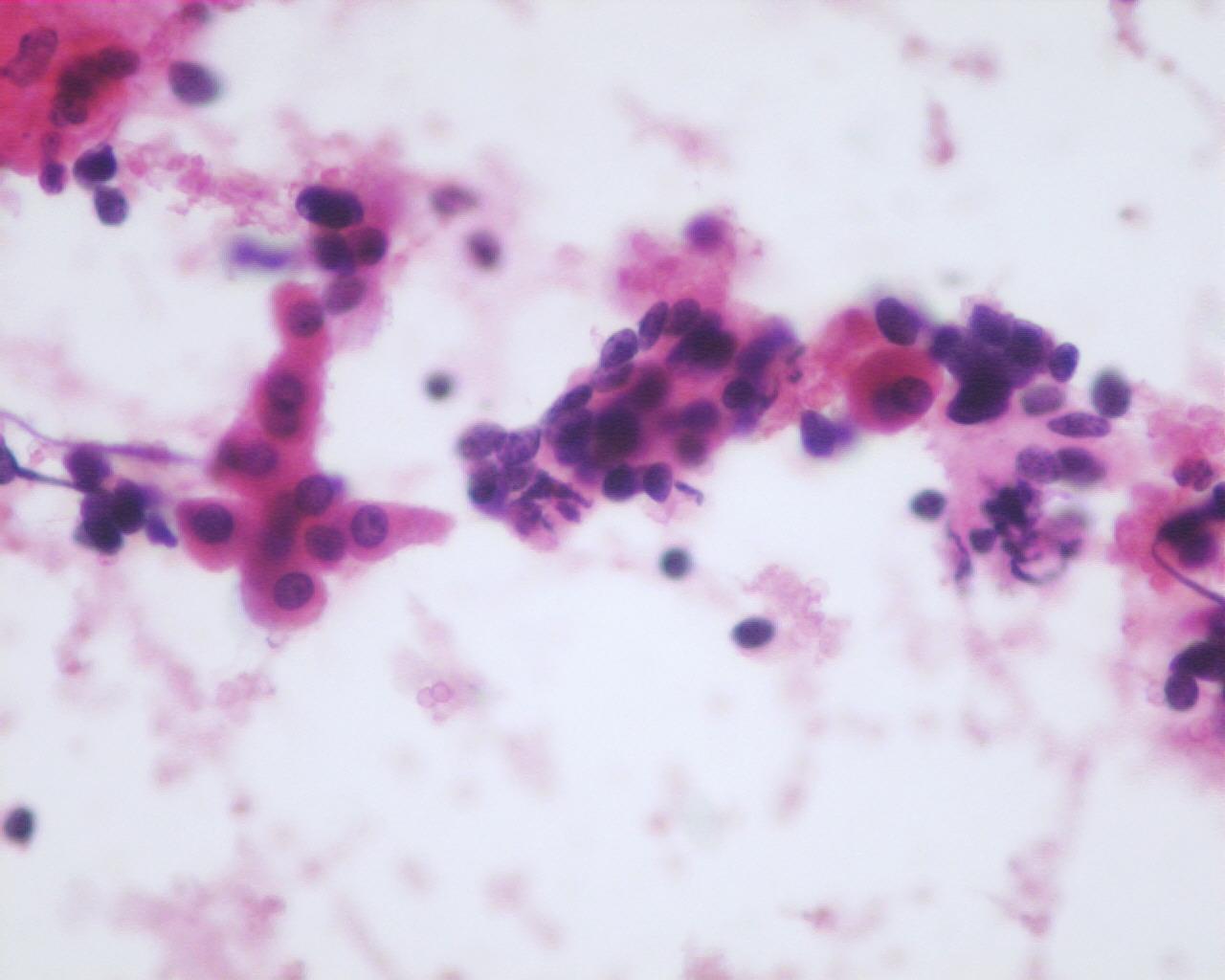
- Sparse to moderate granular cytoplasm (depends on the degree of differentiation)
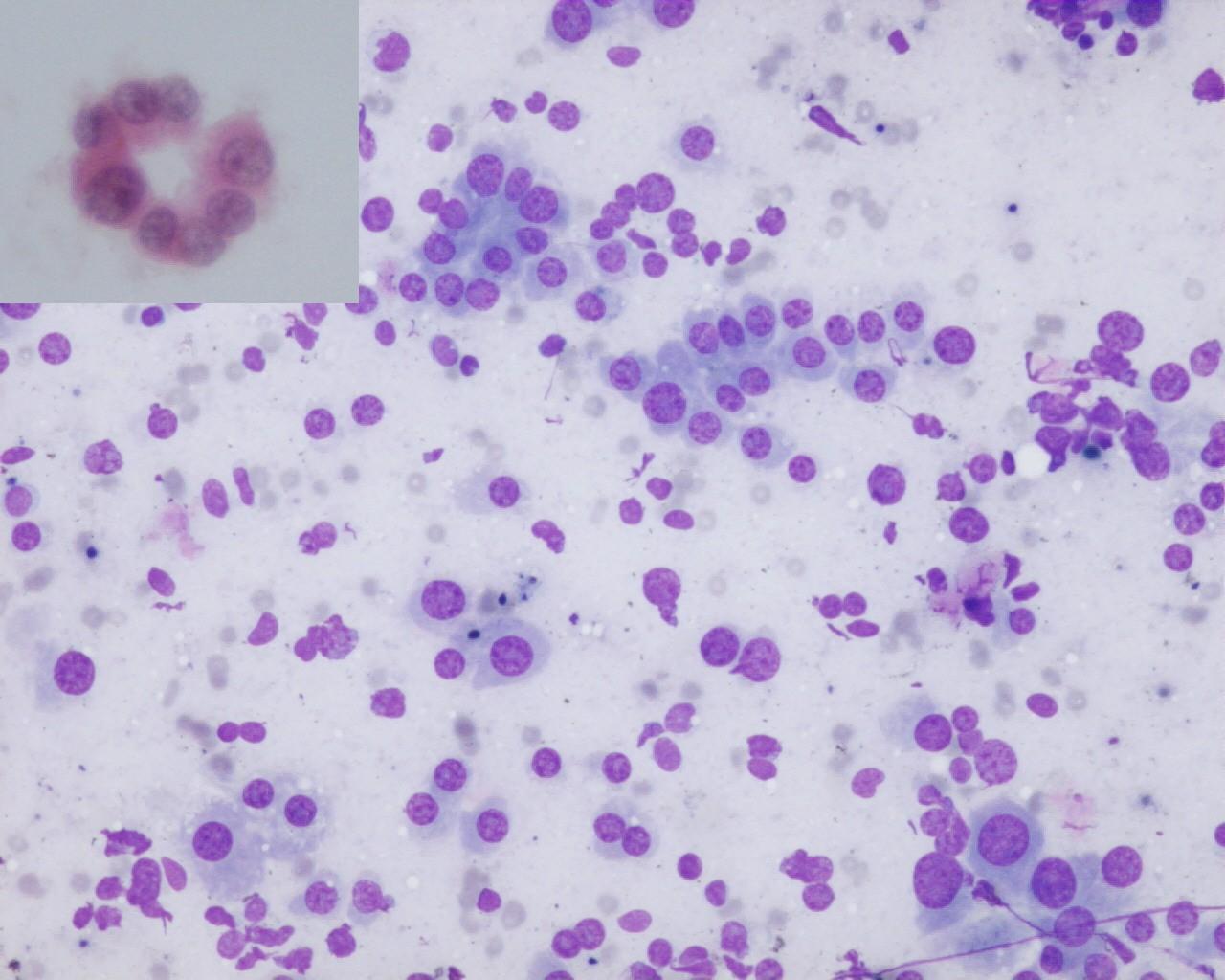
- Cells occur singly or in trabeculae, acini, cords and rosettes (anaplastic subtype)
- Nuclear moulding (anaplastic subtype)
- Nuclear pyknosis
- Hematopoietic elements (more frequent in the foetal subtype)
- Mesenchymal elements: osteoid
Immunocytochemistry
- Low molecular weight cytokeratin’s: positive
- Alpha-fetoprotein: positive (75%); may be negative in anaplastic subtype
- EMA: positive (except for the anaplastic subtype)
- CEA: positive, with canaliculus staining pattern (except for the anaplastic subtype)
- Chromogranin A: positive (focal) (50%)
- HepPar1: positive
- Vimentin: positive (75%); generally negative in anaplastic subtype
- HCG: positive (giant cells)
- glypican 3: positive
- HMB45: positive (occasionally)
- CD99: positive
- CD56 (NCAM): positive
- Neuroendocrine markers: positive
- NB84: positive
- Bcl-2 : positive
- Desmin: positive
- CD45: negative
- Desmin: negative (except in teratoid tumours)
Genetic studies
- No consistent pattern of chromosomal anomalies
- P53 gene mutation
Differential diagnosis
- Hepatocellular carcinoma
- Differential diagnosis with the embryonic and macrotrabecular subtypes
- Rare under three years of age
- If present, is usually associated with previous hepatitis B infection, cirrhosis or metabolic diseases
- In well-differentiated forms, there are great similarities between these entities, and distinguishing them is very difficult
- Vimentin: negative
- Metastatic Yolk sac tumour
- May present hepatoid differentiation
- Eosinophilic hyaline globules in intra or extracellular locations (visceral yolk sac differentiation)
- Single cells or in spherical or papillary aggregates
- Rhabdomyosarcoma
- Other components of hepatoblastoma are not present
- Muscular markers: positive
- Small round blue cell “metastatic” tumours, e.g. neuroblastoma , Wilms’ tumour, lymphoma, Ewing’s sarcoma (Fig 79)
- This may be a problem, especially in anaplastic subtypes
- Small morphological details can help: rosettes, fibrillary background, tubular formation, mainly isolated cells, lymphoglandular bodies, dark and light cells, etc.
- Immunocytochemistry may give a clue to the diagnosis
Main points
- Embryonal tumour derived from pluripotent hepatic stem cells
- High incidence of trisomy 20 and trisomy of all or part of chromosome 2
- Main prognostic factor: complete resect ability
- Other prognostic factors: tumour size, stage and multifocality
- Foetal type is the only histological subtype that leads to changes in therapy regarding stage I tumours
- Distant metastasis in 20% of the patients at diagnosis
- Five-year survival rate is 75%