Clinical features
- Most common non-rhabdomyosarcomatous soft tissue sarcoma
- 15-30% of soft tissue malignancies in the first two decades
- Painless tumours are generally localized around large joints (80% knee and ankle)
- Involvement of the synovial membrane is very rare ( 10% )
- Head and neck and mediastinum (less frequent)
- Focal calcification (30%)
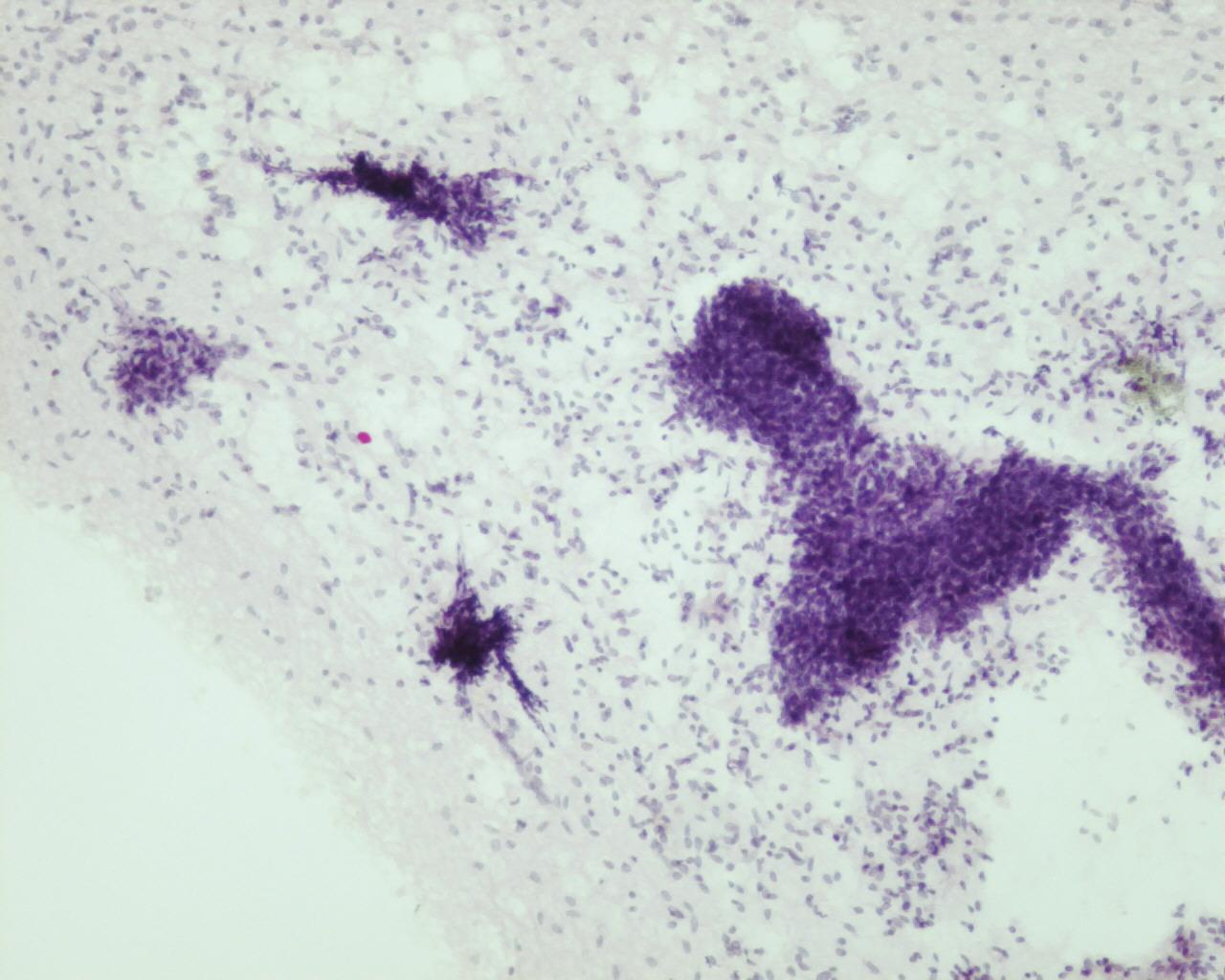
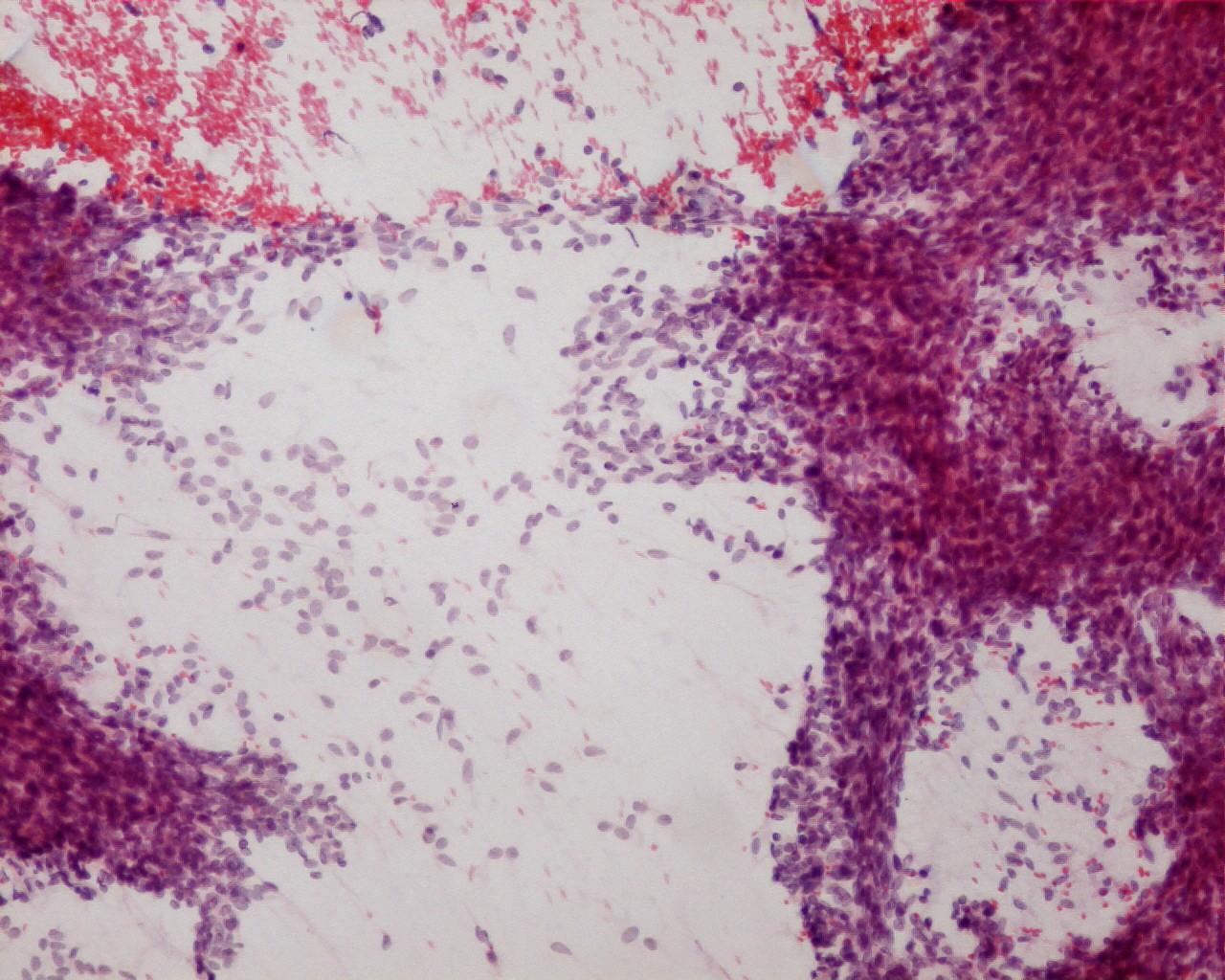
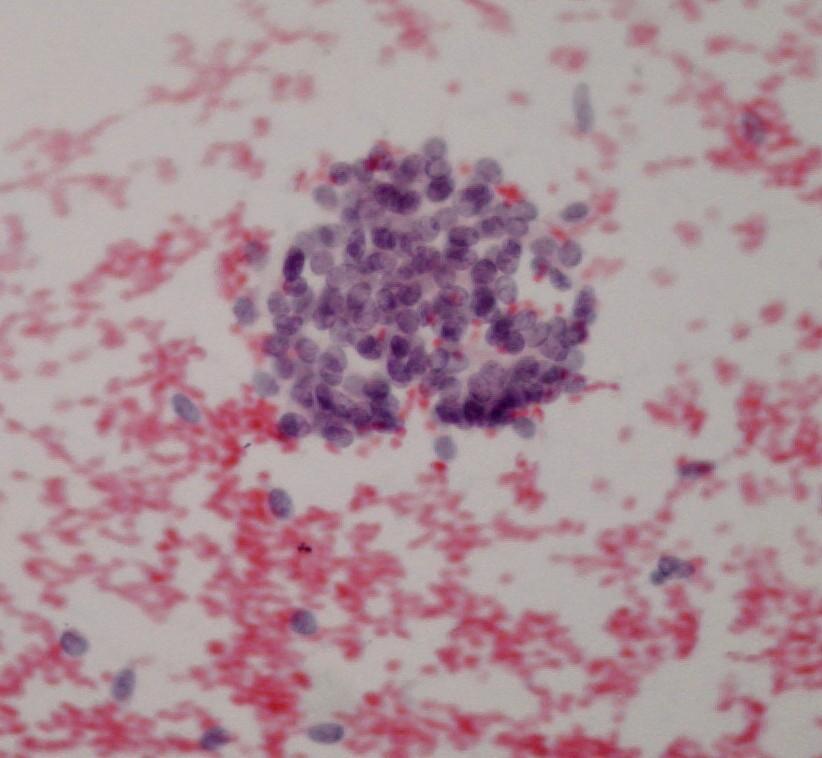
Fig 40 – Synovial sarcoma- Dispersed stripped nuclei, single spindle-shaped cells and cell-tight tissue fragments (H&E). Remark in the bottom right a cohesive epithelioid
- Hypercellular smears
- Cell-tight tissue fragments with irregular borders with a vascular network
- Dispersed single spindle-shaped cells
- Typical non-pleomorphic cells
- Single, hyperchromatic round or oval nuclei
- Inconspicuous nucleoli
- Scant to abundant cytoplasm
- Stripped nuclei
- Recognition of a biphasic pattern (epithelial and spindle) is of a great help
- Myxoid background matrix or basement membrane ( hyaline globules) and cholesterol crystals
- Mast cells
- Variants: undifferentiated small round cells; pleomorphic cells or rhabdoid
Immunocytochemistry
- Monophasic spindle pattern
- Mucin : Positive
- Vimentin: Positive
- EMA: Positive (even in cases negative to other keratins)
- Keratins: Positive, mainly high molecular weight cytokeratins (60-70%)
- CD99: Positive in 50-100% of cases and in both spindle or poorly differentiated pattern (absence of membranous pattern)
- Bcl-2: Positive (79%)
- S-100 protein: Positive (30-60%)
- CEA: Negative
- CD34: Negative
- CD56-NCAM: Negative (even in poorly differentiated pattern)
- Desmin: Negative
- WT1: Negative
- Biphasic pattern:
- Low weight cytokeratin : Positive
- AE1/AE3: Positive- also positive in poorly differentiated pattern
- EMA: Positive (95%) – also positive in poorly differentiated pattern (42%)
- Bcl-2: Positive- also positive in poorly differentiated pattern
Electron microscopy
- Glandular formation
- Desmosome-like junctions
- Micro Lumina and microvilli
Genetic studies
- t(X; 18) (p11.2; q11.2) – (90%) (specific)
- t(X; 18) (p11.21; q11.2) – occasionally
Differential Diagnosis
- Fibrosarcoma of Infancy
- Differential diagnosis with monophasic synovial sarcoma is a challenge and most of the times impossible without immunohistochemical studies or genetic studies (see Fibrosarcoma of Infancy) – Morphology by its own is not a clue.
- Malignant peripheral nerve sheath tumour
- 50% associated to neurofibromatosis Type I
- Pain during aspiration
- In the dependence of a large peripheral nerve
- Wavy appearance of nuclei (unreliable)
- Cytokeratins: Negative
- Lacks t(X;18)(p11;q11)
- Hemangiopericytoma
- Not a common diagnosis in children
- In children, they are generally subcutaneous
- Cytomorphologic overlap
- Common pattern to many neoplasms
- According to some authors, this diagnosis in cytology should be avoid
- “Small round cell Tumours” ( e.g. Ewing sarcoma)- in poor differentiated synovial sarcoma
- See small round cell tumours
- Rhabdomyosarcoma/Rhabdoid tumour ( in poor differentiated synovial sarcoma)
- See rhabdomyosarcoma and rhabdoid tumour.
- Epithelioid sarcoma and extrarenal rhabdoid tumour ( in poor differentiated synovial sarcoma)
Main points
Diagnosis of Synovial sarcomas is easy to achieved, if both epithelial and spindle patterns are present. In monophasic spindle subtypes cytological diagnosis can be suggested and should be confirmed with immunohistochemical studies and genetic studies. Careful attention should be given to clinical and imagiologic features.
- 5 year survival is 50-70%
- Adverse clinical outcome: 10-50% metastasize mainly to the lungs, pleura, bone or regional lymph nodes
- Prognostic factor- criteria of Increased risk of tumour relapses: Age, size (>5cm), histological grade, Rhabdoid pattern 6, poorly differentiated areas, neurovascular invasion; p53 over expression; high Ki67 proliferation index, necrosis, presence of metastasis.
- Local recurrence is exceptional if excision is wide.