Clinical features
- Adipose tissue tumours represent 6% of soft-tissue tumours in paediatric age and lipoblastomas represent 30%
- 88% of the cases occurs under 3 years
- More common in boys, in extremities (38-73%), trunk, retroperitoneum (10%), mediastinum and chest
- Association with malformations, seizures or development delay
- Recurrence has been reported in up to 25% of cases
- Deep-seated tumours can give symptoms related to compression of adjacent organs
- When infiltrative grow, it is called lipoblastomatosis
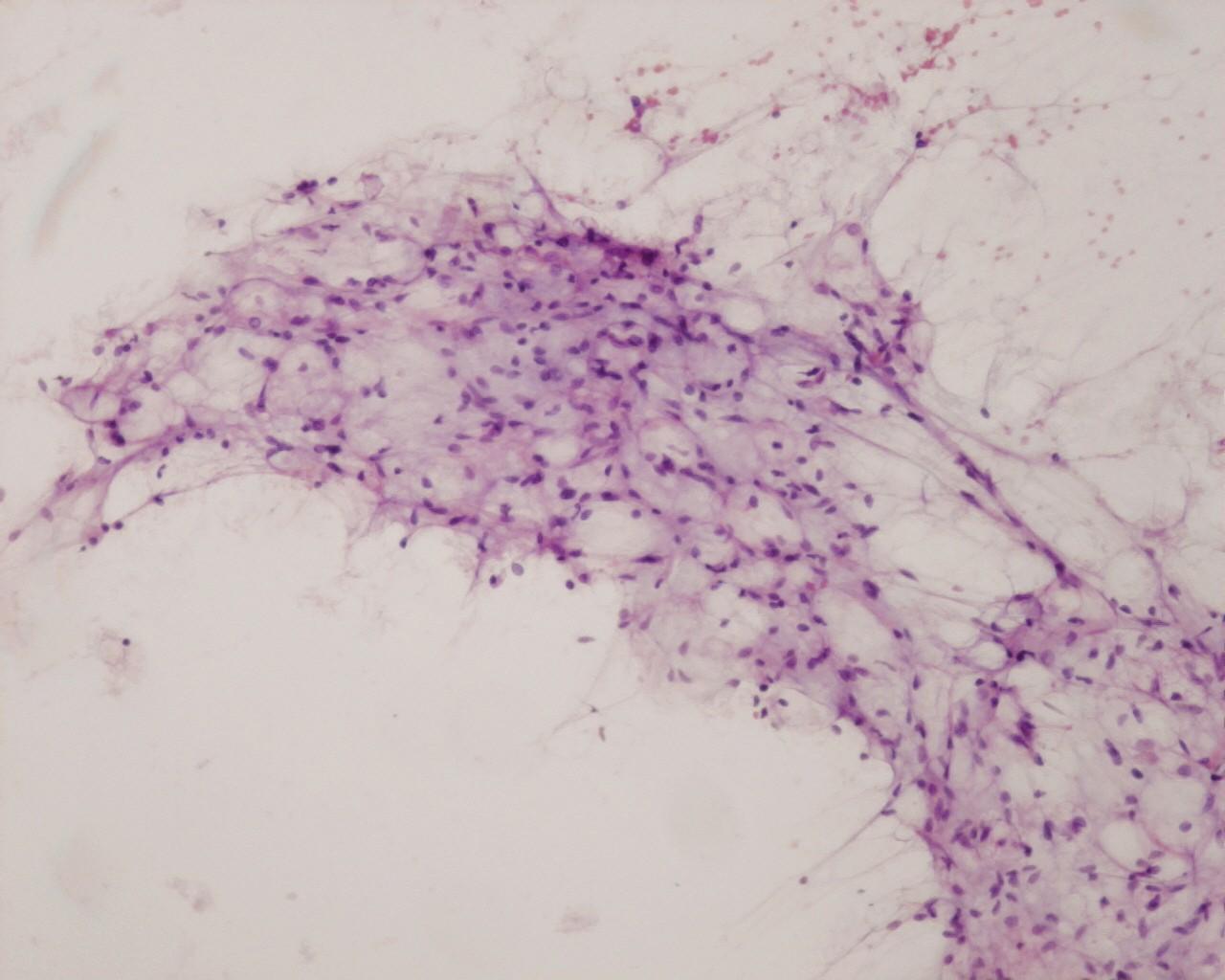
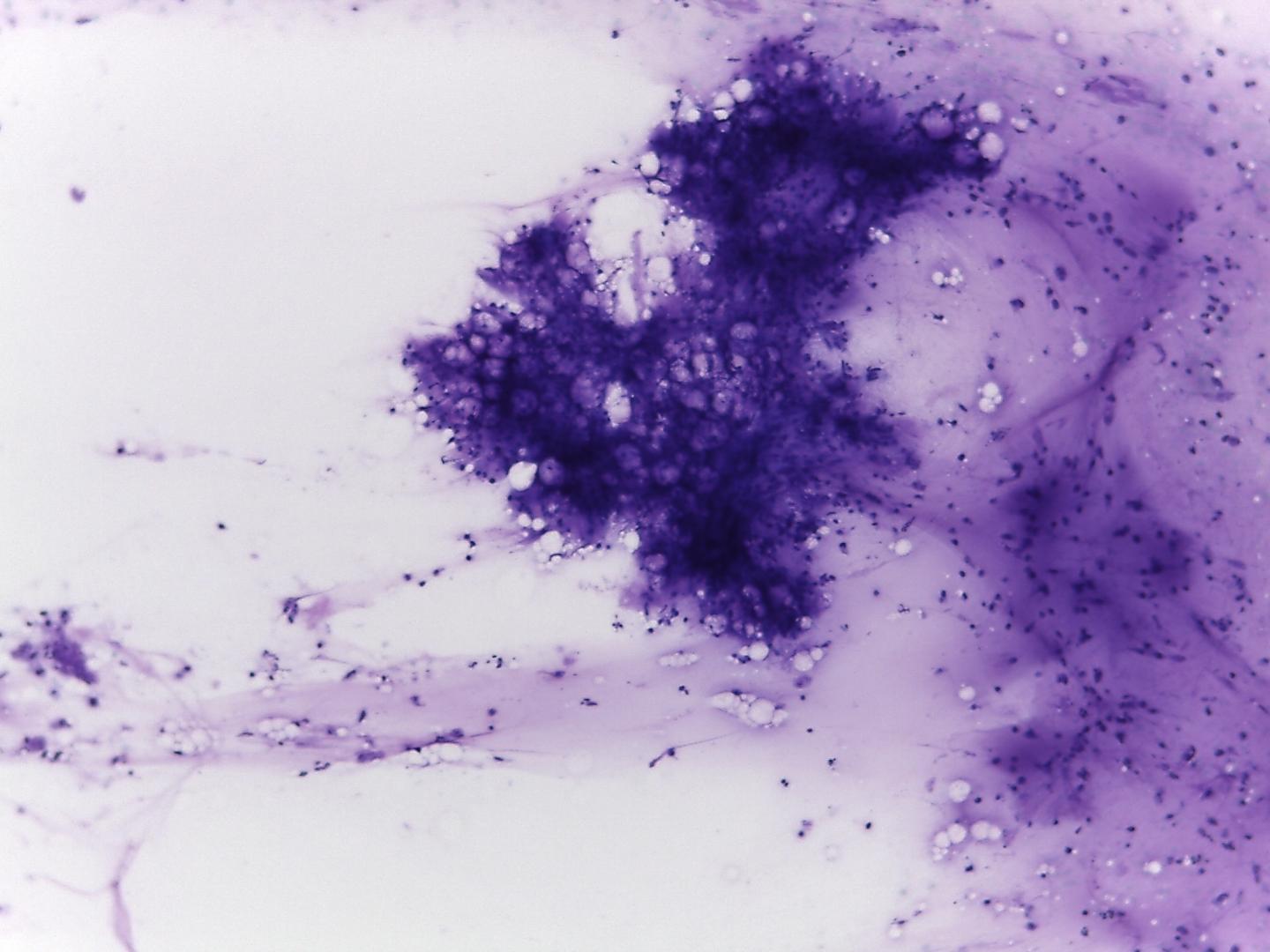
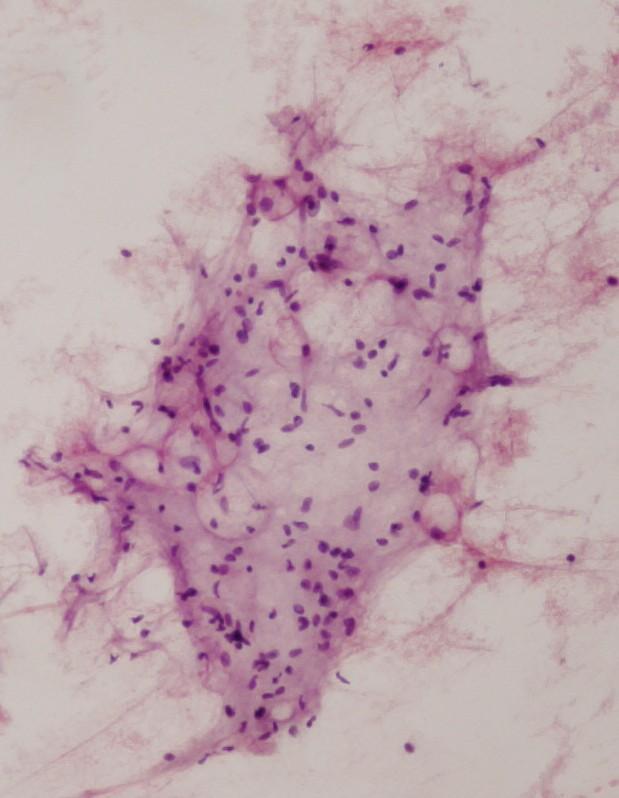
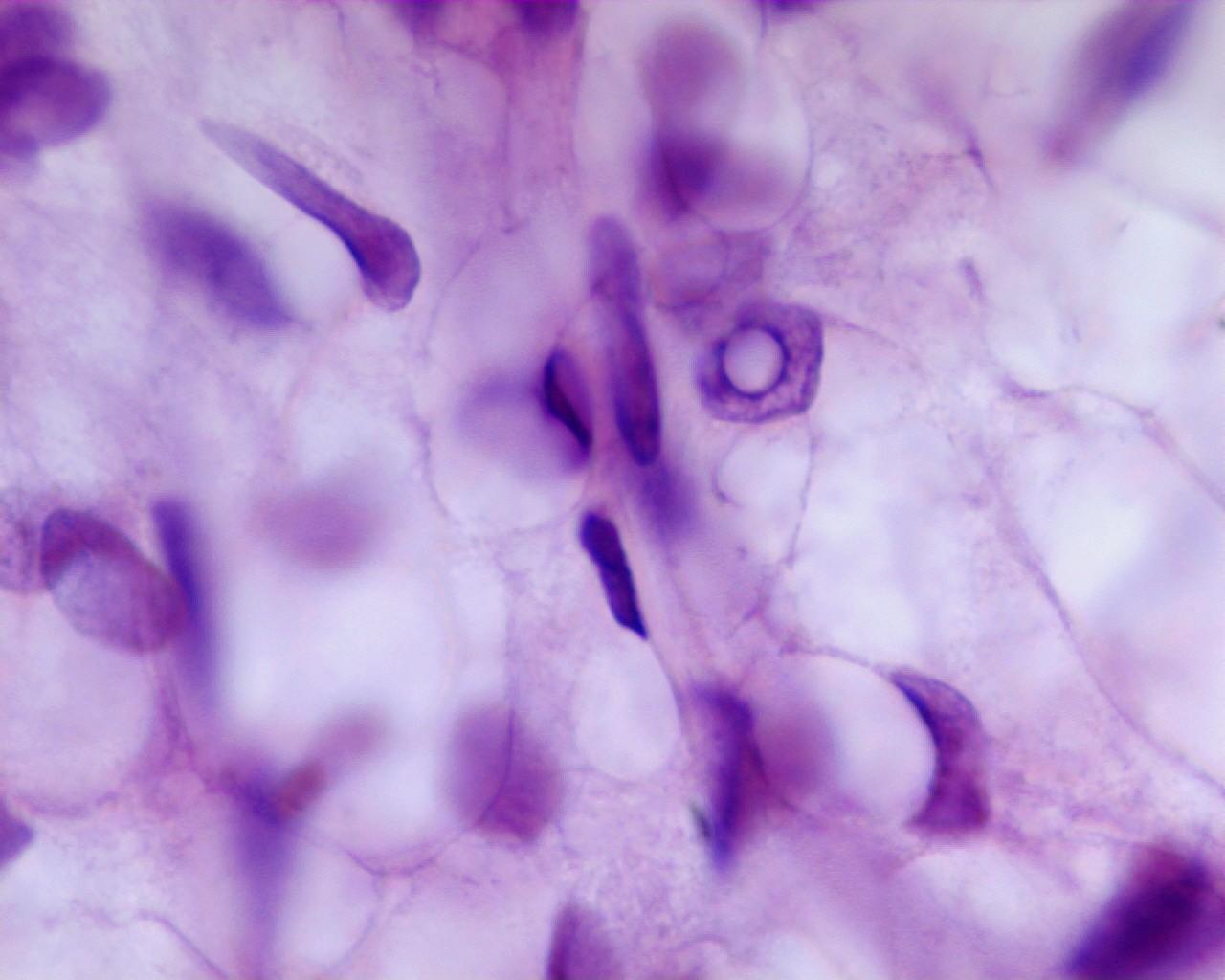
Fig 18a (H&E), Lipoblastoma – Fragments of adipose tissue, (mixture of fat cells in different stages of maturation) (H&E)
- Myxoid background
- Fragments of myxoid stroma, sometimes mixed with adipocytes
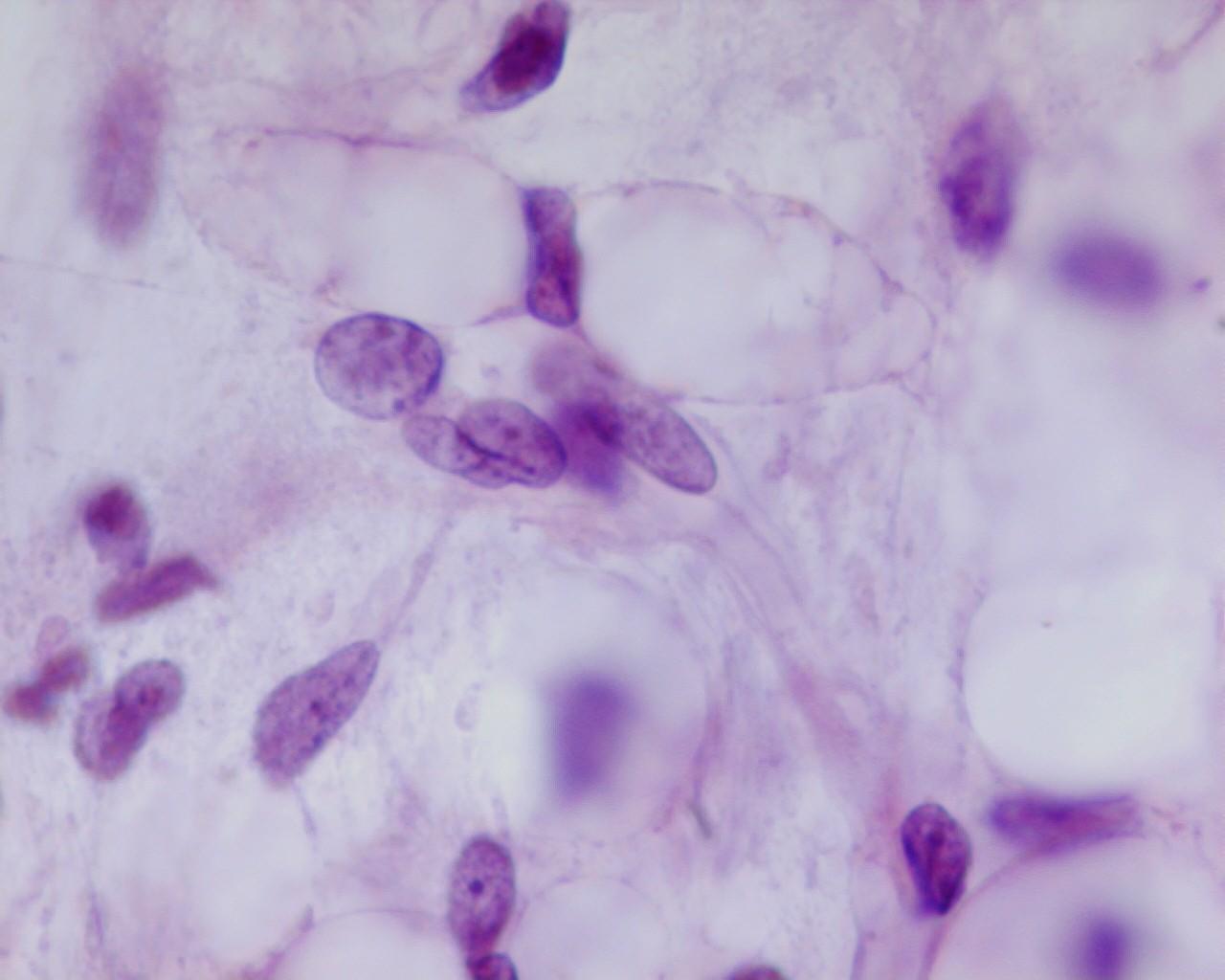
- Fragments of adipose tissue, with a mixture of fat cells in different stages of maturation (central or eccentrically placed nucleus )
- capillary network is usually present
- Mesenchymal immature cells
- Cells with delicate chromatin
- Nucleoli absent
- Lipoblasts without nuclear polymorphisms
Genetic Studies
- Structural rearrangements involving chromosome 8q11-13 region
Differential Diagnosis
Numerous paediatric lesions can have adipose tissue within:
- Liposarcoma Myxoid (distinction in FNAC is sometimes difficult)
- Rare lesions in children
- Atypical lipoblasts
- Atypical univacuolated cells
- Abundant characteristic myxoid background
- Branching capillaries are prominent
- chromosome rearrangements in the region of 12q14
- Intramuscular haemangioma
- Skeletal muscle
- Mature adipocytes
- No atypia
- Intramuscular lipomas
- Atrophic muscle fibbers
- Mature adipose cells
- Nephroblastoma
- Located in the kidney
- Presence of mesenchymal, blastemal or epithelial differentiation
Main points
- Lesions mature as time passes
Surgery is the treatment of choice