This content is also available in:
Español
Čeština
Magyar
Polski
Malignant mesothelioma
Malignant mesothelioma arises most commonly in the pleura and rarely in the peritoneum. The occurrence of this tumour is related to asbestos exposure. The tumour grows as multiple plaques and large nodules on the serosal surface. Most patients have an effusion at the time of presentation. The effusion is often bloody; if not, it has the colour and consistency of honey.
Clinical history of mesothelioma
- Asbestos exposure
- Persistent pleural effusions
- Chest pain
- Dyspnea
- Evidence of pleural thickening
Histologic classification
- Epitheliod
- Sarcomatoid
- Mixed (biphasic)
The epithelioid type, which is the most common, can show different growth patterns: tubular, papillary, microcystic, solid, adenomatoid, decidual, pleomorphic, clear cell, small cell. A desmoplastic variant of mesothelioma is also described.
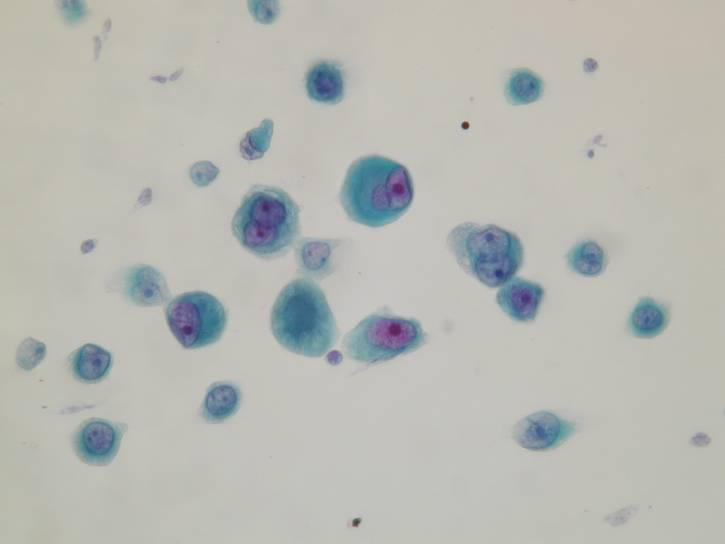
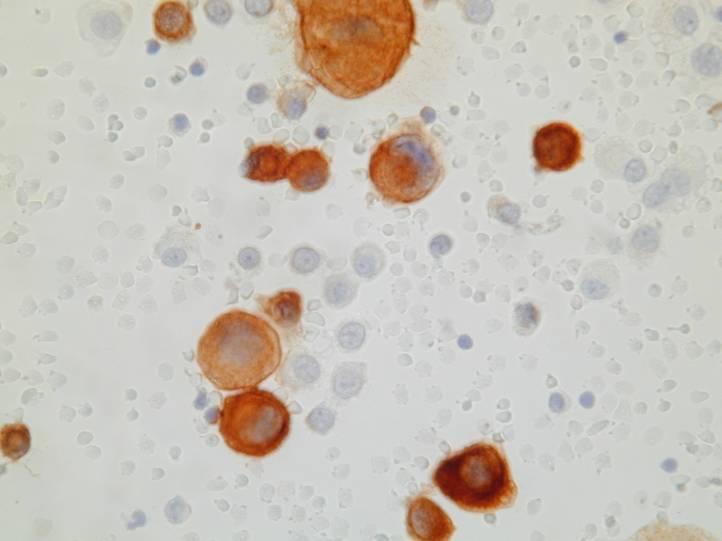
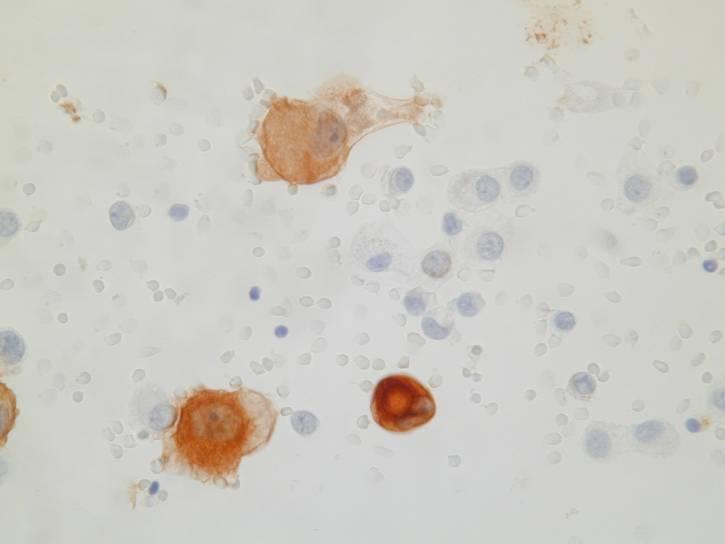
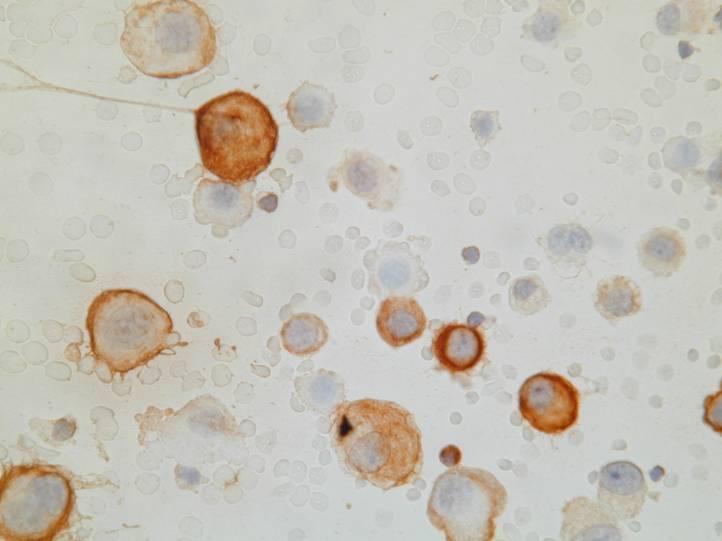
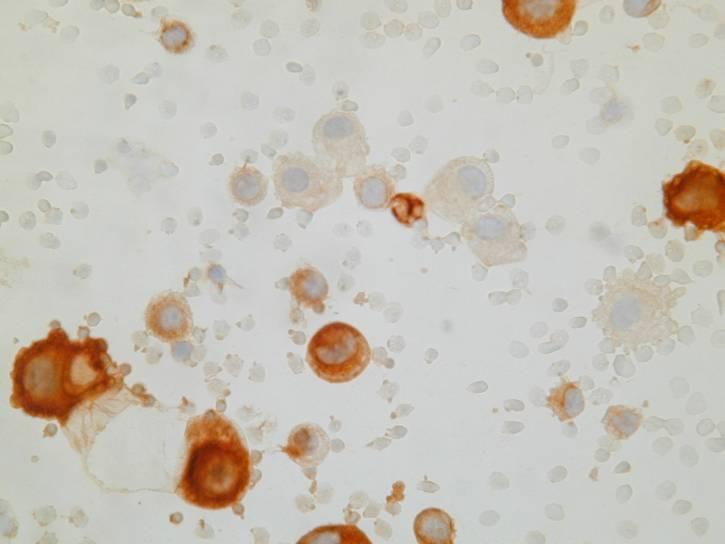
Cytologic diagnostic features
- Large clusters with scalloped (knobby) edges
- Cytomegaly
- Round, centrally placed nuclei
- Prominent nucleoli
- Binucleation and multinucleation
- Dense cytoplasm with peripheral halo
- Normal N/C ratio
- ‘Windows’
The most common pattern, seen in the epithelial type, consists of numerous large clusters, sometimes showing branching, composed of up to several hundred of cells. The cells are usually recognizably mesothelial in origin and in most cases larger than normal mesothelial cells. Nuclear atypia is mild in most cases. On cell block sections, the clusters are a solid mass of cells, or they may contain a collagenous or mucopolysaccharide core. Rarely, the cells form lumina.
Some fluids show different patterns. They can be sparsely cellular and composed of lymphocytes only. Sometimes the neoplastic cells are predominantly dispersed rather than in clusters.
Uncommon cytologic features
- Predominantly isolated tumour cells
- Lymphocytes only
- Tumour cells with abundant obscuring lymphocytes and histiocytes
- Psammoma bodies
- Cytoplasmic vacuolization
Many initial effusions from patients with mesothelioma are negative for neoplastic cells. The diagnosis is more difficult when uncommon patterns are observed, such as when the tumor cells are predominantly dispersed or obscured by an abundant lymphohistiocytic infiltrate.
Differential diagnosis
- Reactive mesothelial cells
- Metastatic tumors
- Adenocarcinoma
- Squamous cell carcinoma
- Epithelioid hemangioendothelioma
Major differential problems in mesothelioma
- Reactive mesothelial hyperplasia vs. epithelioid mesothelioma
- Fibrous pleuritis vs. desmoplastic mesothelioma
- Epithelioid mesothelioma vs. secondary carcinoma
Reactive vs. neoplastic mesothelial cells
- Cellularity
- Frequency of multinucleation
- Size of macronucleoli
- Average cell size
- N/C ratio
- Nuclear membrane
- Intranuclear inclusions
- Cytoplasm staining
- Clusters vs. non cohesive cells
- Glycogen content
- Background
Pitfalls
- When is an atypical mesothelial cell malignant?
- Use most criteria not just few
- Rarely all criteria will be fulfilled
- Beware of scanty cellular specimens
- Check thickness of clusters
- Double check PAS positive inclusions
To increase accuracy in distinguishing benign from malignant mesothelial cells, other methods of analysis can be useful in cases in which a mesothelioma is suspected, including flow cytometry and cytogenetic analysis, or fluorescence in-situ hybridization on liquid based preparations. Cytogenetic analysis, which is very sensitive and specific, can detect clonal cytogenetic aberrations indicative of malignancy.
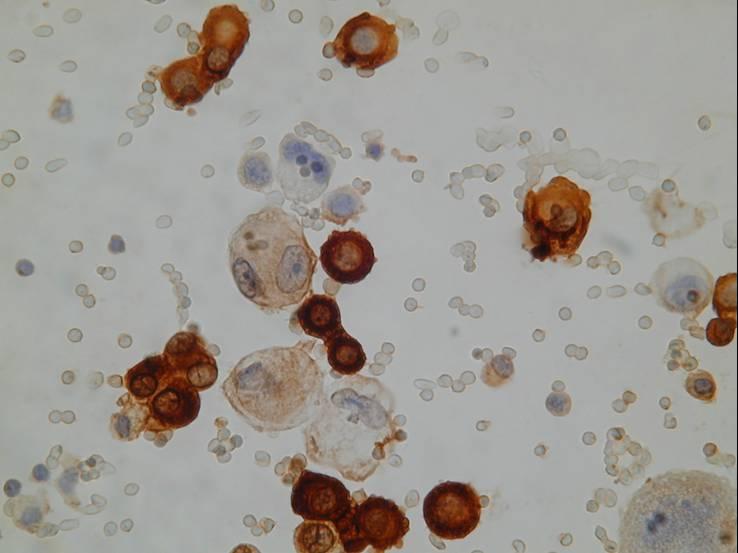
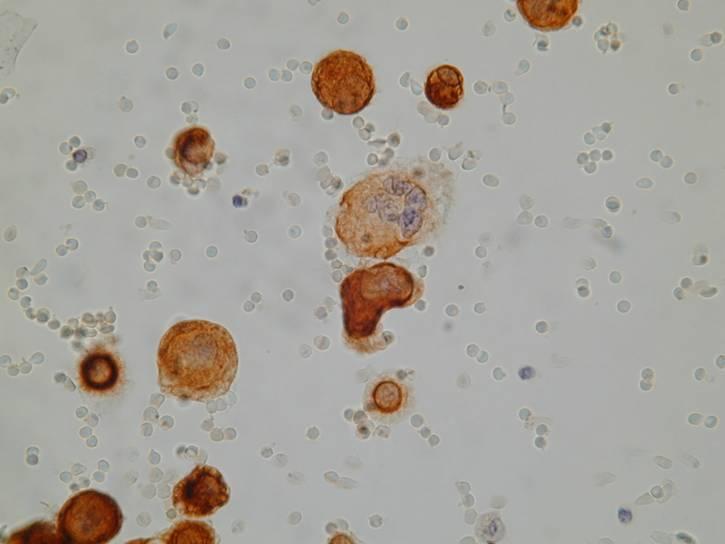
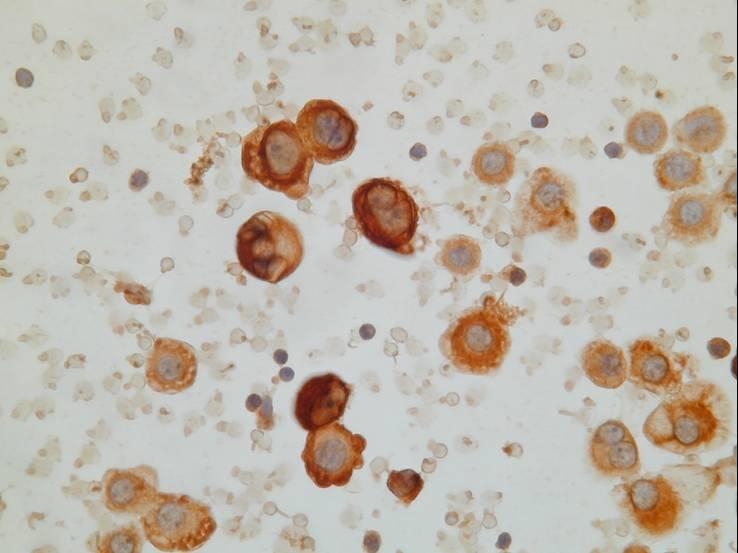
Mesothelioma can be hard to distinguish from adenocarcinoma (particularly when the cells have a vacuolated cytoplasm). In mesothelioma the tumor cells usually form a morphologic continuum with benign-appearing mesothelial cells, differently from adenocarcinoma cells. Mesothelial cells are often separated by slit-like windows. On cell block sections, a core of collagen and stromal cells surrounded by neoplastic cells is more commonly seen in mesothelioma than in adenocarcinoma, whereas ring-like structures with hollow cores are seen in some adenocarcinomas. A scalloped rather than smooth edge to the clusters is characteristic of mesothelioma. Morphologic features are often not able to provide an unequivocal identification.
The distinction can be made in almost all cases by using histochemical (PAS, DPAS and Mucicarmine) and immunocytochemical stains.
Primary vascular tumours of the lung (angiosarcomas, hemangioendotheliomas), can spread to the pleura, and can also mimic mesothelioma, particularly epithelioid hemangioendothelioma. However, they are positive for vascular markers (CD31, CD34) and negative for mesothelial markers like Calretinin and WT1.