This content is also available in:
Čeština
Türkçe
Reporting terminology
Diagnostic terminology for pancreatic FNA used empirically a five-tier system including the following categories:
- Negative for malignant cells
- Atypical cells present
- Suspicious cells present
- Positive for malignant cells
- Non-diagnostic specimen
A negative diagnosis in the setting of a radiologically detected mass implies either a failure to sample the lesion or the presence of a benign process such as chronic pancreatitis. An atypical diagnosis reflects a mild degree of cytologic atypia, often in the setting of inflammation. This interpretation implies a low suspicion of malignancy. A diagnosis of suspicious cells present implies a strong suspicion of malignancy, but the cytologic features are insufficient for a definite diagnosis.
The non-diagnostic category is used when lesional tissue was not obtained or the cells are obscured beyond interpretation; it is accompanied by an explanation, such as obscuring inflammation or blood, air-drying artefact, or insufficient cellularity. Although no adequacy criteria exist for pancreatic FNA, a non-diagnostic interpretation due to the lack of epithelial cells may also be appropriate in the setting of cysts and pseudocysts. When the imaging and cytologic features suggest either a mucinous cystic neoplasm or an intraductal papillary mucinous neoplasm, without definite features of malignancy, the most appropriate diagnosis is consistent with a mucinous cystic (or an intraductal papillary mucinous) neoplasm.
All cytology samples are microscopically described and attributed to one of five categories (C1-C5) similarly to what is done in other institutions and for other anatomical sites when issuing diagnostic cytology reports 10,11: C1, non-diagnostic; C2, negative; C3, atypical; C4, suspicious; C5. The C1, non-diagnostic category is used when it is clear that lesional tissue was not obtained and/or there is insufficient cellularity overall. Material that is suboptimal for evaluation such as cells obscured by blood or inflammation or cells exhibiting poor preservation precluding further assessment can also be interpreted as non-diagnostic. A negative interpretation (C2) implies a benign process; nonetheless, in some instances there does exist the possibility of a malignancy that has not been sampled. The C3, atypical category is used when the degree of cytological and/or architectural atypia is mild, often in the setting of inflammation, previous duct instrumentation, or sparse cellularity. As mentioned previously it is also used in those cystic lesions where malignancy cannot be ruled out by cytology alone. This implies a low suspicion of malignancy, although malignancy cannot be entirely excluded. The C4 category implies a high likelihood of malignancy, but the degree of cytological atypia is quantitatively or qualitatively insufficient for a definitive diagnosis of malignancy; a benign reactive process cannot be entirely excluded. Representative examples of each category are illustrated in Figure 2. During 2011, 114 pancreatic FNA samples were examined at Imperial College with the following distribution: C1, (17.5%); C2, 27 (23.7%); C3, 20 (17.5%); C4, 7 (6.1%); C5, 40 (35.1%). The cases were also received from other hospitals who do not have access to direct assessment of the specimens by a BMS. In the same year 115 cases of biliary brushings were examined with the following distribution: C1, 3 (2.6%); C2, 75 (65.2%); C3, 16 (13.9%); C4, 13 (11.3%); C5=8 (7%). These results indicate a higher likelihood of cancer in pancreatic FNAs compared with biliary brushings and a greater likelihood of the cytology being diagnostic rather than suspicious. The percentage reported as C3 was similar, but the reasons for this category are different: brushings are more likely to be non-specific atypical while pancreatic FNAs diagnosed as C3 may represent specific low-grade neoplastic lesions.
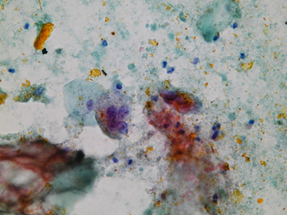
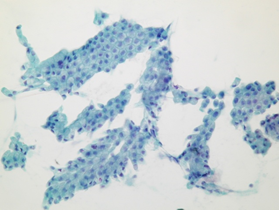
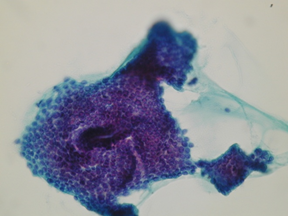
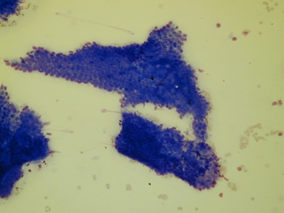
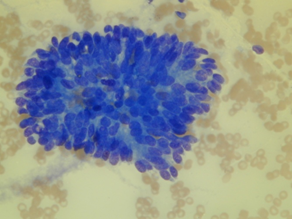
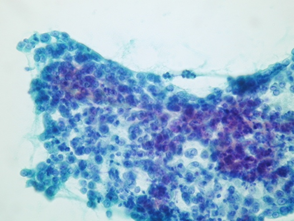
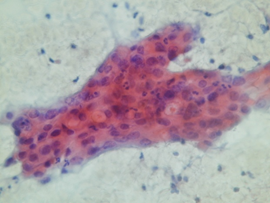
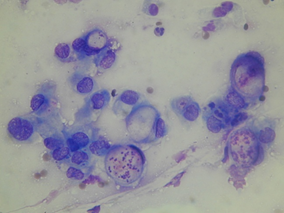
Examples of cytological categories C2-5. (a) A Pseudocyst with biliary pigment, crystals, multinucleated histiocytes and debris, no epithelial cells were to be seen (C2). (b) Bland ductal cells without background mucin (C2). (c, d) Papanicolaou- (c) and May-Grünwald Giemsa (MGG)-stained (d) slides showing sheets of bland ductal cells associated with mucin in a case of surgically proven intraductal papillary mucinous neoplasm (C3). (e) Cohesive groups of epithelial columnar cells showing mild crowding and only minimal nuclear atypia (C4). (f) Groups of cohesive but more pleomorphic epithelial cells with prominent nucleoli in a acute inflammatory background (C4). Both cases turned out to be ductal adenocarcinomas of low grade. (g, h) Papanicolaou- (g) and MGG-stained (h) slides showing markedly atypical and mucin secreting cells in crowded groups and singly dispersed with signet-ring features (C5).
The proposed terminology scheme by the Papanicolaou Society (ref) has 6 categories (Table 2).New and somewhat controversial is the category Neoplastic that is divided into clearly benign neoplasms and other neoplasms. Interpretation categories do not have to be used, but some pathology laboratory information systems require them, and such categorization may aid in clinical and translational research.

