This content is also available in:
Čeština
Cystic tumors
Pancreatic cystic tumors account for about 5% of pancreatic neoplasms. They also include cystic dilatations of intraductal neoplasms, cystic degenerations of solid neoplasms (solid-pseudopapillary tumor), and solid neoplasms with focal cystic change (ductal adenocarcinoma with cystic degeneration, cystic acinar cell carcinoma, cystic pancreatic endocrine tumor).
Serous cystadenoma
It usually occurs in elderly women, most often in the body and tail of the pancreas. It is usually benign, although rare cases of serous cystadenocarcinoma have been reported. Star-burst calcifications within a central scar can be diagnostic on imaging when present. Most tumors are ‘microcystic’ with multiple, <2cm cysts, but can be unilocular due to specific variant or due to haemorrhagic degeneration, causing problems with imaging diagnosis.
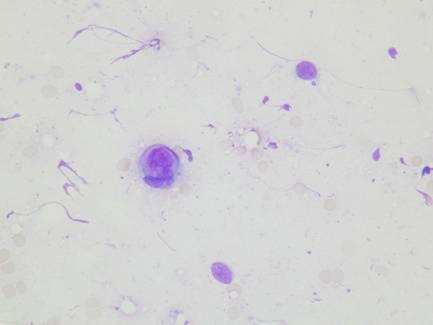
Cytologic preparations are characterized by low cellularity and the cells are arranged in small clusters or flat sheets. The cytoplasm is clear or vacuolated and the nuclei are small and round. The presence of glicogen is demonstrated by PAS positivity.
Cytologic diagnostic features
- Watery, non-mucinous fluid
- Scanty cellularity
- Clean, proteinaceous or bloody background
- Monolayered sheets or small, flat clusters
- Bland, uniform, round nuclei
- Scanty but visible non-mucinous cytoplasm
Differential diagnosis
- Benign ductal or acinar epithelium
- Lymphangioma/hemangioma
- Mucinous cystic neoplasm
- Cystic pancreatic endocrine tumor
- Metastatic renal cell carcinoma
Mucinous cysts of the pancreas
WHO classification
- Mucinous cystic neoplasm
- Mucinous cystadenoma
- Borderline mucinous cystic neoplasm
- Mucinous cystadenocarcinoma
- Intraductal papillary mucinous neoplasm
- Intraductal papillary mucinous adenoma
- Intraductal papillary mucinous neoplasm of borderline malignancy
- Intraductal papillary mucinous carcinoma
- Intraductal papillary mucinous neoplasm with invasive carcinoma: tubular type or colloid carcinoma
Mucinous cystic neoplasms
They usually arise in women in the fourth and fifth decades, mostly in the pancreatic tail. They encompass a spectrum ranging from benign to low malignant potential to frankly malignant. The cytomorphology of mucinous epithelium does not reliably predict biologic behaviour.
They are lined by mucinous epithelium which is generally non-papillary, but can also be focally papillary. In women they can show a subepithelial ‘ovarian-like’ stroma. The cysts do not communicate with the pancreatic ductal system and may contain thin septae.
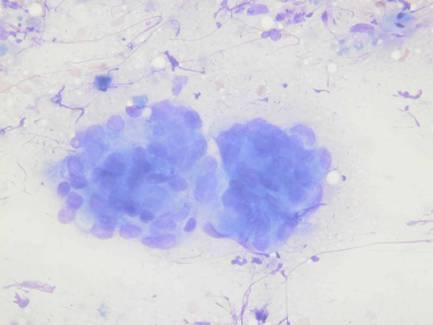
Cytologic diagnostic features
- Abundant background mucin and muciphages
- Columnar mucinous cells in sheets, papillae and single cells
- Varying degrees of nuclear and architectural atypia
- Nuclear pseudostratification
- Nuclear enlargement, crowding or overlapping
- Complex papillary groups
Both intra- and extracellular mucin are highlighted by a mucicarmine stain.
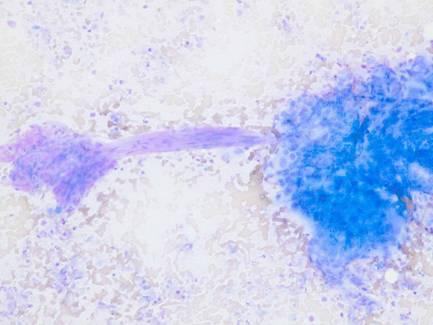
Mucinous cystadenocarcinoma – cytologic diagnostic features
- High cellularity
- Abundant background mucin
- Increased cellular dyshesiveness
- Marked nuclear atypia (enlargement, anisonucleosis, macronucleoli)
- Signet ring cells
- Numerous mitoses
- Necrosis

Intraductal papillary mucinous neoplasm
This tumor is characterized by a primarily intraductal growth and its cytomorphology encompasses a spectrum ranging from benign to frankly malignant. It may grow diffusely along the entire length of the duct and its branches, or form focal complex papillary proliferations. The cytologic features are similar to those of mucinous cystic neoplasms. Necrosis, mitoses and marked nuclear atypia lead to a diagnosis of papillary mucinous carcinoma.

