This content is also available in:
Italiano
Español
Čeština
Magyar
Polski
The types of epithelial cell seen in a cervical smear are determined by:
- The degree of maturation of the cervical epithelium
- The location of the squamocolumnar junction
- The presence of metaplastic change in the cervix
- The stage in the menstrual cycle when the smear is taken
- Several basic cytological patterns can be recognised
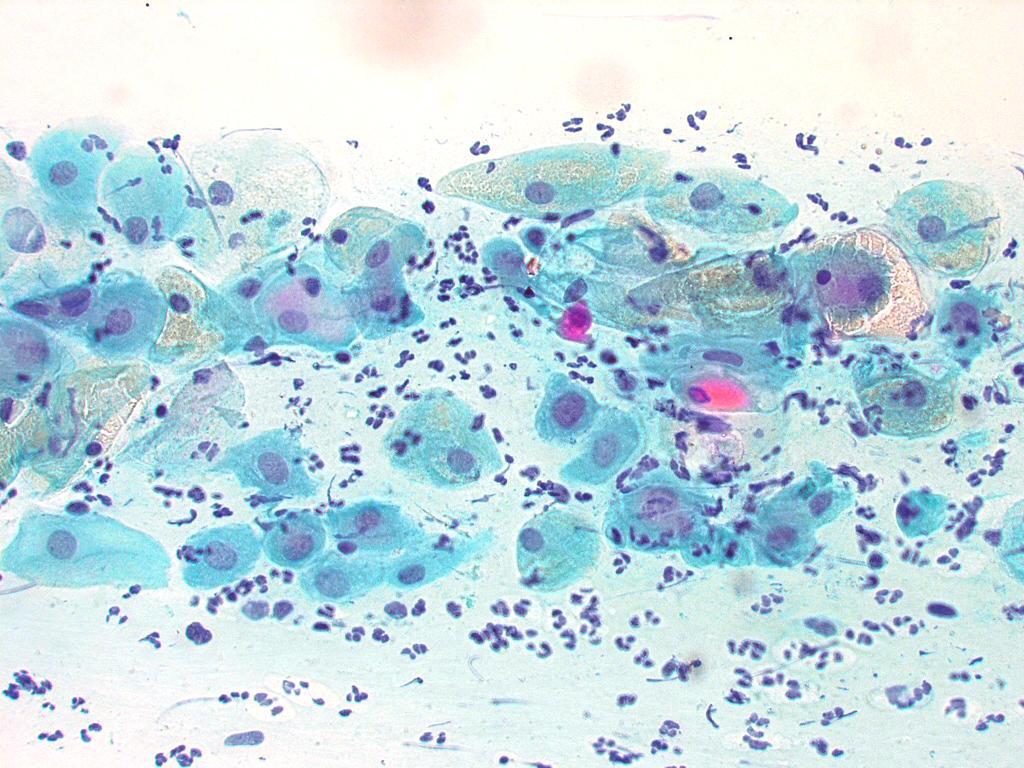
Under the influence of unopposed oestrogen the squamous epithelium of the cervix thickens and a smear taken mid cycle for example will contain numerous superficial squamous cells. In practice, however most smears show an intermediate level of maturation probably reflecting endogenous progestogens or exogenous hormones administered as oral contraceptives.
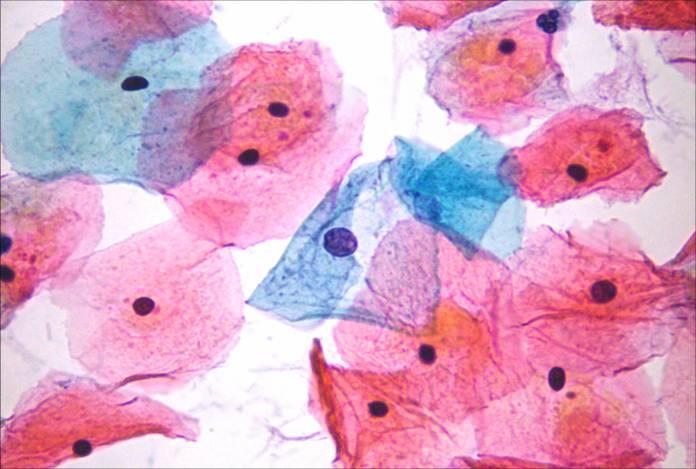
The position of the squamocolumnar junction varies. After the menopause it recedes into the endocervical canal beyond the reach of the Ayre spatula. Thus smears taken after the menopause rarely contain endocervical cells. Smears taken in the presence of ectropion contain abundant endocervical cells. Immature metaplastic cells are found usually in young women of child bearing age. They are rare in smears from older women.

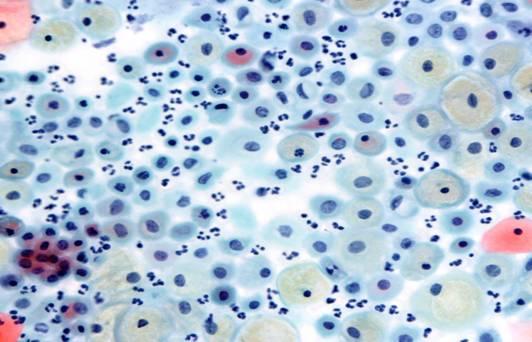
Daily smears taken throughout the menstrual cycle reflect variation in the maturity of the cervical epithelium. Smears taken just before the onset of menstruation will contain intermediate cells and possibly some navicular cells. Endometrial cells may be found in smears during menstruation or during the first 10 days of the cycle. Smears should not be taken during menstruation as the heavy blood staining obscures the squamous cells. Their presence at any other time may have pathological significance. For example endometrial cells in a well oestrogenised smear from a post menopausal patient suggests endometrial pathology and further investigation of the patient.
The cytological pattern of a smear in pregnancy is that of an intensified progesterone effect with clustering and folding of the intermediate cells which become packed with glycogen and rounded (the so called navicular cells). Doderlein bacill may cause a marked cytolysis so that cytological interpretation is unreliable. Smears taken up to 6 week post partum reflect the absence of circulating hormones and appear atrophic with large glycogen packed parabasal type cells.
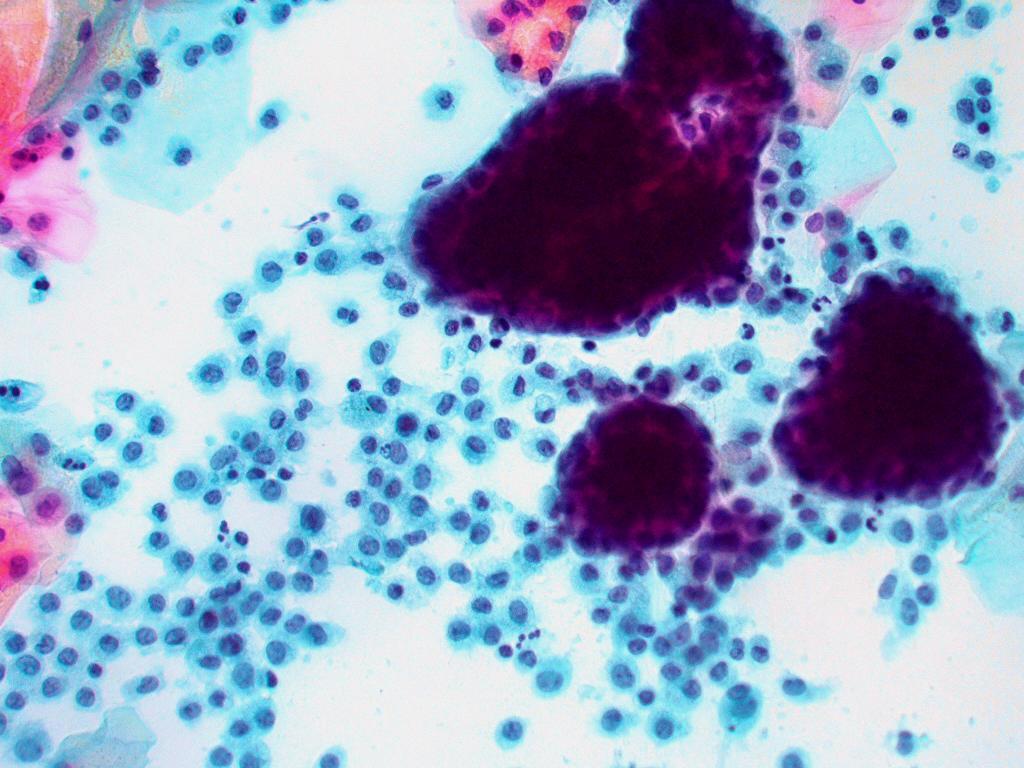
The menopause is associated with diminishing oestrogen activity which is reflected in the smear pattern. This can only be recognised when oestrogen activity is greatly reduced and the premenopausal multilayered epithelium is replaced by the thin epithelium of a post menopausal woman. Smears usually contain scanty parabasal cells either as discrete rounded cells or as sheets of cells. Free nuclei may be abundant. As the smear is thin, the cells may dry before the smear is fixed so that cell morphology may be poorly preserved. Infection is common. It is difficult to identify endocervical cells in post menopausal smear as they may be out of reach of the spatula. A cervical brush specimen may be advisable in these case. Dense basophilic mucus plugs may be found in these smears. When diagnosis is in doubt it may be useful to administer a short course of oestrogen therapy to the patient and repeat the smear with in 10 days when a low proliferative pattern may be seen.